Incisional Biopsy of Oral Tumors
Sarah Boston, DVM, DVSc, DACVS, ACVS Founding Fellow of Surgical Oncology, ACVS Founding Fellow of Oral & Maxillofacial Surgery, VCA Canada, Newmarket, Ontario, Canada

Technique
Histopathology of oral tumors is often preferred (over cytology) because it can help provide a definitive diagnosis and prognostic information. One study reported good agreement between cytology and histopathology for oral tumors1; however, incisional biopsy is preferred because either sedation or anesthesia is needed for complete oral examination with either tumor aspiration or biopsy in most patients.
Shaving off an oral tumor for simultaneous diagnosis and treatment is not recommended (see Common Mistakes When Diagnosing & Treating Oral Tumors). Intralesional or marginal excision does not result in successful long-term control of most oral tumor malignancies, and because oral mucosa heals quickly, the original tumor location can be difficult to discern once the tumor is cytoreduced to microscopic disease, complicating definitive treatment with surgery or radiation (Figure 1).
COMMON MISTAKES WHEN DIAGNOSING & TREATING ORAL TUMORS
Performing cytology via fine needle aspiration rather than histopathology via biopsy in a sedated or anesthetized patient
Histopathology is recommended for definitive diagnosis.
Performing an excisional biopsy (ie, shaving off the tumor), as the biopsy site will heal quickly, making definitive resection with margins difficult
Incisional biopsy should be performed and the tumor kept intact so appropriate margins can be determined.
Biopsy of maxillary tumors through the skin overlying the maxilla, as this can compromise reconstruction in a combined-approach maxillectomy
Biopsy should be obtained via the mouth directly over the tumor.
Not taking digital images and performing a biopsy when an oral tumor is discovered during dental prophylaxis
Failing to consider oral neoplasia as a differential in patients with unexplained tooth loss or loose teeth in one area of the mouth, especially in geriatric cats
Biopsy should be performed in the oral cavity without traversing the skin (Figure 2). In cases of malignancy, the biopsy tract is contaminated with tumor cells and should ideally be removed via definitive resection. Biopsy should, therefore, be performed through tissue that will be removed if excision is performed. For tumors of the maxilla, biopsy through overlying skin can complicate reconstruction techniques after combined-approach maxillectomy.
In combined-approach maxillectomy, a bipedicle flap is created with the skin of the upper lip to access the dorsal maxilla via full-thickness skin incision along the muzzle, caudal to the nasal planum, and to access the intraoral maxilla via incision along the labial gingiva (Figure 3).2 Biopsy performed through the skin of the upper lip can compromise the flap used for reconstruction, negatively impacting cosmetic appearance and tumor control.
A wedge or punch biopsy may not be feasible for a hard mass that arises from the maxilla or mandible; digital radiography or CT can be used to help plan the biopsy approach (Figure 4). A Jamshidi needle can be used for bone biopsy if bone is involved, and small rongeurs can be used to biopsy deep tissues.
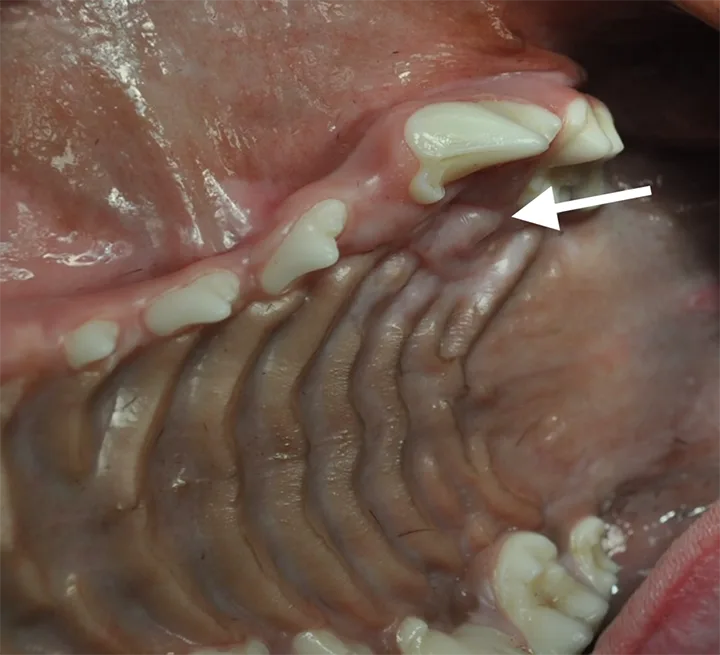
FIGURE 1
Right caudal maxillary fibrosarcoma 2 weeks after being shaved off via excisional biopsy. Scarring is present at the level of 109 (buccal surface; arrow), but it is difficult to discern the original dimension of the mass.
Additional Diagnostics
Biopsy can be performed alone or in combination with other diagnostic procedures. Digital images should be taken for the medical record and potential referral. Mandibular lymph nodes should be palpated and/or aspirated for cytology. If malignancy is suspected, 3-view thoracic radiography should be performed to rule out metastatic disease.
In a specialty clinic, oral mass biopsy is often combined with CT for local and distant staging to help guide surgical planning. In many cases, an oral tumor is diagnosed in a primary care clinic during dental prophylaxis, an ideal time to perform a biopsy. Squamous cell carcinoma in cats can be subtle early in the course of disease and may mimic dental disease. Abnormal areas of osteolysis or masses should be biopsied at the time of dental prophylaxis.
Diagnosis
Histopathologic diagnosis can vary from a benign (eg, inflammatory, hyperplastic) to a malignant lesion.3 A survey of oral biopsy specimens identified benign tumors (29.1%), hyperplastic lesions (24.1%), inflammatory lesions (14.7%), and malignant tumors (32.1%) in dogs and benign tumors (4.8%), hyperplastic lesions (15.1%), inflammatory lesions (57.5%), and malignant tumors (21.9%) in cats.3 A survey of common diagnoses of oral masses in dogs and cats in a dentistry specialty clinic reflected a higher percentage of neoplasia; malignant tumors (37%), tumors of odontogenic origin (34%), and inflammatory lesions (28%) were reported in dogs, and inflammatory lesions (51%) and squamous cell carcinoma (37%) were most commonly reported in cats.4 A study reporting incidence of oral malignancy in a veterinary teaching hospital found that 53.6% of canine oral tumors were classified as malignant (25.4% were benign) and 58.1% of feline oral tumors were classified as malignant (2.5% were benign).5 Incidence of oral tumors in both dogs and cats was 0.5%.5
Common differential diagnoses in dogs with oral tumors include malignant melanoma, osteosarcoma, fibrosarcoma, squamous cell carcinoma, and odontogenic tumors. Squamous cell carcinoma is the most common oral neoplasm in cats.3,4
Treatment & Outcome
Definitive diagnosis of oral malignancy often leads to surgical treatment, with the goal of removing the tumor and ≈1 cm of adjacent normal tissue, including soft tissue and bone. The mass is more likely to be small with earlier diagnosis, possibly resulting in lower morbidity, improved cosmesis and function, and better oncologic outcome. Oral tumors should be biopsied immediately after they are noted by the pet owner or clinician to determine diagnosis. Watching and waiting is rarely a good strategy and can result in poor outcomes in cases of malignancy, as most owners do not know what to watch for. Malignant oral tumors are more difficult to manage locally as they progress and can metastasize to distant sites.
Step-by-Step: Oral Incisional Biopsy
What You Will Need
Sterile surgical gloves
Sterile gauze
Oral chlorhexidine solution
Metzenbaum scissors
Tissue forceps
Sterile suture pack
Needle drivers
3-0 or 4-0 monofilament absorbable suture
Suture scissors
Step 1
Heavily sedate or anesthetize the patient. Wipe the oral cavity with sterile oral chlorhexidine solution (optional).
Step 2
Remove a 5- to 10-mm diameter tissue specimen using an intraoral approach directly over the mass.
Author Insight
Preference can determine which instruments are used. Wedge biopsy requires a scalpel and forceps; punch biopsy requires a punch biopsy (6-10 mm), forceps, and Metzenbaum scissors or a scalpel. Jamshidi needle biopsy may be required for masses that involve bone.
A punch biopsy or wedge biopsy technique can be used for most oral masses, depending on clinician preference. Tissue specimen size depends on mass size. Biopsy should be performed on the central portion of the mass to avoid disrupting and contaminating normal surrounding tissues.
Step 3
Close the biopsy site, if possible, with 3-0 or 4-0 monofilament absorbable suture.
Author Insight
Digital pressure should be applied to control bleeding. The wound should be allowed to heal by second intention if the mass is too firm or too friable to allow biopsy site closure. Owners should be advised there may be a small amount of bleeding that should resolve in ≈24 hours.