Image Gallery: Transtracheal Wash Cytology
Kyle Webb, DVM, DACVP, ANTECH Diagnostics, Orlando, FL
A transtracheal wash is a fairly simple method for collecting samples from the airways for cytologic evaluation. It involves instilling saline into the lower trachea and subsequently retrieving the fluid, with the goal of obtaining cells from the trachea and bronchial tree. These cells can then be viewed microscopically to detect possible airway disease, including inflammation, infection, and neoplasia.
Transtracheal wash is a minimally invasive technique for sampling larger airways (eg, trachea, mainstem bronchi). Although bronchoalveolar lavage is superior in cases of lower airway or interstitial lung disease, transtracheal wash can be performed on patients without anesthesia, offering an advantage over bronchoalveolar lavage.
Transtracheal washes can be grouped into several broad categories based on the types and proportions of cells identified: suppurative (septic and nonseptic), eosinophilic, hemorrhagic, and neoplastic. Categorizing transtracheal washes allows clinicians to narrow the list of differential diagnoses.
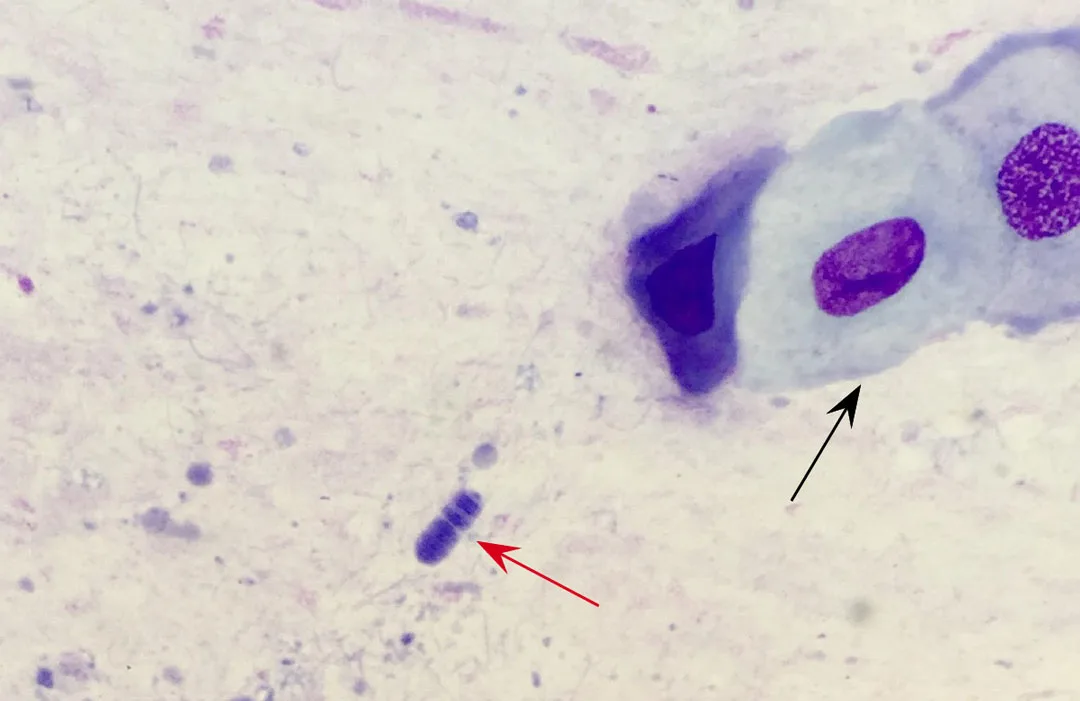
Figure 1
Oropharyngeal contamination resulting from improper sampling technique is a common problem with transtracheal wash cytology. The presence of uniform squamous epithelial cells (black arrow) alongside oral bacterial flora, such as Simonsiella spp as pictured here (red arrow), indicates oropharyngeal contamination. Simonsiella spp can be recognized by their pathognomonic morphology that resembles a pill capsule with internal striations (ie, “stacked coin” appearance). Modified Wright’s; 600x total magnification