Hypercalcemia in Dogs and Cats

ProfileDefinitions
Hypercalcemia is defined as either an elevation of total serum calcium (tCa) or ionized calcium (iCa) above physiologically normal homeostatic levels.
In dogs, tCa above 12.0 mg/dl or iCa above 1.5 mmol/L qualifies as hypercalcemia.
In cats, tCa above 11.0 mg/dl or iCa above 1.4 mmol/L qualifies as hypercalcemia.
Elevated iCa can affect multiple organs, resulting in altered cell membrane permeability and subsequent disturbances in biological functions of the nervous, gastrointestinal, cardiac, and renal systems.
Causes of hypercalcemia are diverse, but may be categorized into several subgroups differentiated by severity and underlying cause.
Nonpathologic increases in serum calcium are often incidental findings and do not result in clinical signs classically associated with severe elevations in calcium. Causes accounting for nonpathologic hypercalcemia include:
Mobilization of calcium secondary to skeletal growth, most commonly observed in young large- to giant-breed dogs
Lipemic serum samples resulting in spurious elevations in calcium.
Increases in serum calcium may be transient, often resulting from significant but reversible dehydration or relative increases in intravascular protein concentrations, especially albumin. Hemoconcentration secondary to any of the following causes may result in transient hypercalcemia:
Gastrointestinal fluid loss associated with excessive vomiting, diarrhea, and/or salivation
Renal fluid loss related to primary or secondary polyuria with concurrent inadequate compensatory polydipsia
Loss of intravascular volume into a body cavity such as the peritoneal, pleural, or pericardial space, resulting in a state of relative dehydration.
PathophysiologyAlthough many causes of elevated calcium levels are benign, hypercalcemia is usually associated with some underlying disease process. Pathologic hypercalcemia may be categorized as parathyroid hormone (PTH)-dependent or independent as follows:
PTH-dependent conditions-primary hyperparathyroidism results in excessive production of PTH, resulting in elevated iCa.
Neoplastic
Adenoma (common)
Functional adenocarcinoma (rare)
Nonneoplastic
Hyperplasia (rare)
PTH-independent conditions
Many diseases that induce elevations in calcium are not dependent on the production and secretion of PTH per se, but cause hypercalcemia via alternative mechanisms.
Cancer-related
Humoral hypercalcemia of cancer occurs when cancer cells liberate a peptide that is structurally similar to endogenous PTH, called PTH-related peptide (PTH-rp).
Lymphoma (most common form in dogs): anatomical location-mediastinal (common), immunophenotype-T cell (common)
Anal sac apocrine gland adenocarcinoma (second most common form in dogs): tumors cause elevations in calcium through the secretion of PTH-rp.
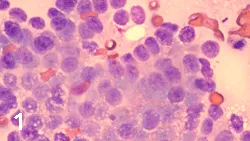
Cytologic sample of an anal sac mass identified upon rectal examination in a 4-year-old, spayed female dalmatian with history of straining to defecate and acute-onset polyuria and polydipsia. Diagnosis of hypercalcemia of malignancy secondary to PTH-related peptide production from apocrine gland anal sac adenocarcinoma was the final diagnosis.
Various types of epithelial cancer (carcinomas): mammary, thyroid, adrenal, pancreatic, pulmonary, nasal, thymic epithelial, bronchogenic (feline), oral squamous cell (feline)• Pathologic elevations of calcium may result from focal or diffuse skeletal osteolysis, whereby direct destruction of the bone matrix by invading tumor cells or associated cytokines results in calcium release. The following types of cancer have been identified to or theoretically could cause hypercalcemia via this described mechanism: T-cell lymphoma; acute lymphoblastic leukemia; multiple myeloma (common); solitary osseous plasma cell tumor; and primary bone sarcomas (rare) including osteosarcoma, fibrosarcoma, chondrosarcoma, and hemangiosarcoma.

An invasive soft tissue mass involving the glossal frenulum of a 13-year old, castrated male domestic shorthair. Screening blood analysis identified pathologic elevations in serum calcium. Histopathologic evaluation of the mass confirmed oral squamous cell carcinoma.
• In very rare instances, hypercalcemia mediated by elevations in PTH-rp has been associated with infectious disease, including that caused by Heterobilharzia americana (dog).- Pathologic hypercalcemia may also result from disorders associated with granulomatous processes. Mechanistically, hypercalcemia is mediated by macrophage dysregulation of 1α-hydroxylase activity, resulting in excessive conversion of cholecalciferol to highly active 1,25-(OH)2 cholecalciferol (calcitriol). Granulomatous diseases documented to be associated with hypercalcemia include the following:• Angiostrongylus vasorum (dog)• Atypical mycobacterium (feline)• Blastomyces dermatitidis (dog)• Cryptococcus neoformans (feline)

Cranial mediastinal mass identified on thoracic radiographs from a 10-year-old, male castrated golden retriever presenting for hypercalcemia. Upon fine-needle aspiration and cytologic evaluation, the mass effect was confirmed to be T-cell lymphoma.
Calcium homeostasis is a complex process orchestrated by an interaction among 3 principal mediators (PTH, calcitonin, and calcitriol) and their target organs (bone matrix, renal tubules, and intestine). Hypercalcemia may result from any one or a combination of the following derangements:• PTH- or PTH-rp-mediated hypercalcemia-physiologic consequences of elevated PTH or PTH-rp include:- Enhanced calcium reabsorption from the distal tubules- Enhanced conversion of calcitriol in the proximal tubules, resulting in greater intestinal resorption of calcium- Enhanced osteoclast maturation and activity resulting in greater bone resorption activities.• Calcitriol-mediated hypercalcemia-physiologic consequences of elevated active vitamin D3 includes:- Enhanced intestinal resorption of calcium- Synergism with PTH to enhance osteoclast maturation and activity resulting in greater bone resorption.

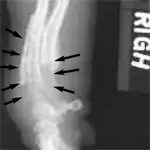
High-detail cervical spinal radiograph of an 8-year-old spayed female, mixed-breed dog, initially presenting for severe neck pain and moderate hypercalcemia. Multiple purely lytic bone lesions are observed throughout the vertebrae and were confirmed to be plasma cell cancer (multiple myeloma).
Causes/Risk/Factors• Hypercalcemia may result from ingestion of toxin containing vitamin D or its active metabolites and has been documented for the following poisons:- Plants that contain calcitriol glycosides (day blooming jessamine)- Rodenticides containing cholecalciferol- Ingestion of antipsoriasis creams containing calcipotriol or calcipotriene.• Miscellaneous causes of hypercalcemia account for a diverse group of processes that cause elevations in tCa or iCa. For the most part, the mechanisms of hypercalcemia associated with these disorders remain poorly defined and include the following:- Idiopathic hypercalcemia (the most common cause of elevated iCa in cats). Most patients do not have any clinical signs.- Chronic renal failure. Associated with elevated tCa but rarely iCa.- Nonneoplastic skeletal disorders. Such disorders as bacterial or fungal osteomyelitis can also result in elevations in calcium.
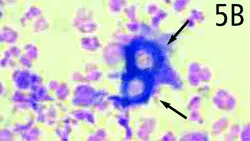
A 5-year-old, castrated male dachshund presenting for chronic lameness, draining cutaneous lesions, and mild hypercalcemia. The radiograph demonstrates a mixed lytic/blastic process involving the distal aspects of the antebrachium (A). Cytologic evaluation of the pathologic bone identified a thick-walled budding organism consistent with Blastomyces dermatitidis (B).
DiagnosisClinical SignsClinical signs associated with pathologic calcium elevations are related to the magnitude of hypercalcemia as well as the rate of elevation. Generally, clinical signs are more pronounced in patients with acute onset of severe hypercalcemia and include the following:• Nervous system- Lethargy and weakness (common)- Neuromuscular twitching (rare)- Seizures• Gastrointestinal tract- Anorexia- Vomiting- Diarrhea or constipation (rare)• Cardiac system- Weakness or collapse- Narrow QT and prolonged PR intervals- Arrhythmias (rare)• Renal system- Polyuria and polydipsia- Dehydration and prerenal azotemia- Renal insufficiency- Calcium urolithiasis
History• Most common pet-owner complaint is excessive urination and thirst.• Clinical onset may be acute or chronic depending on underlying disease process and magnitude and duration of hypercalcemia.• Dogs presenting with primary hyperparathyroidism usually have signs referable to stone disease.
Diagnostic TestsSuggested diagnostic tests to identify causes of hypercalcemia in dogs and cats are listed in Table 1.
Treatment
The urgency for managing hypercalcemia depends on the underlying cause as well as the severity and duration of calcium elevations. The intent of therapy targeting clinical signs is to reverse the deleterious effects of high iCa levels on organ function.• Identification of the underlying cause for hypercalcemia is paramount but should not supersede the immediate supportive care necessary to sustaining and maintain a critically ill patient.• The following supportive care should be instituted immediately:- Vigorous rehydration with isotonic saline (0.9% sodium chloride) or lactated Ringer's solution. Isotonic saline is preferred but not essential-lactated Ringer's solution is a viable option for intravascular volume restoration.• Amount recommended for adequate volume expansion is 100 to 125 mg/kg/day IV- After rehydration, a loop diuretic-most commonly furosemide-may be added to the treatment regimen. Furosemide inhibits the renal membrane Na-K-2Cl cotransporter present in the thick ascending limb of Henle's loop and enhances calciuresis.• Recommended furosemide dosage:Intermittent pulse therapy: 2-4 mg/kg Q 8-12 H IV, SC, or POContinuous-rate infusion: 0.66 mg/kg loading dose followed by a constant-rate infusion of 0.66 mg/kg/hr (equivalent to 5-6 mg/kg Q 8 H)- Sodium bicarbonate (although rarely used) is effective for rapidly reducing iCa levels and should be considered for severely compromised patients.• Recommended sodium bicarbonate dosage: 1 mEq/kg IV slow bolus- Injectable aminobisphosphonates, such as pamidronate, have been shown to be safe and effective for treating dogs and cats with hypercalcemia.• Recommended pamidronate dosage:In cases of vitamin D toxicosis in dogs-1.3-2.0 mg/kg IV over 20 minutes or 2 hours.In cats for management of hypercalcemia-1.0-1.5 mg/kg IV over 2 hours- Calcitonin plays only a minor role in calcium regulation but can reduce serum calcium levels by reducing osteoclast activity and formation and has been used effectively for managing vitamin D toxicosis in dogs.• Recommended calcitonin dosages: 4-6 IU/kg SC Q 8-12 H- Glucocorticoids should be avoided unless a definitive diagnosis has been made, as hypercalcemia secondary to lymphoma is the most common cause of elevated calcium levels in dogs and administration of glucocorticoids before diagnosis of lymphoma can confound or preclude a definitive diagnosis.• Recommended glucocorticoid dosages:Prednisone: 1.0-2.2 mg/kg Q 12 H IV, SC, or PO;Dexamethasone: 0.1-0.22 mg/kg Q 12 H IV, SC, or PO
Follow-UpPatient MonitoringThe intensity and frequency of monitoring hypercalcemia is dictated by the clinical severity of disease. Recommended monitoring in critically ill patients may include the following:
Repeat iCa measurements Q 12 to 24 H with therapeutic adjustments as indicated
Precautions: monitor serum electrolytes in addition to calcium. Aggressive fluid diuresis and loop diuretics may result in hypokalemia.
Course:
Provide adequate time for normalization. Patients with severe hypercalcemia will probably require several days of intensive management before hospital discharge.
After patient stabilization:
Diagnose and treat underlying cause of hypercalcemia
Provide supportive or definitive treatment depending on the cause of hypercalcemia.
In GeneralRelative CostManagement of hypercalcemia can be costly because critically ill patients require intensive hospitalization, diagnostic testing to determine the underlying cause, and treatment.• $$$$-$$$$$ (depending on disease severity and underlying cause)
Costs of therapy for managing hypercalcemic patient (30-kg dog):
Intravenous fluid therapy with hospitalization: $-$$/day
Furosemide therapy: $/day
Sodium bicarbonate: $/day
Pamidronate: $$-$$$/treatment cycle (every 7-28 days)
Calcitonin: $-$$/day
Glucocorticoids: $/day
Prognosis
The outcome for dogs and cats diagnosed and treated for hypercalcemia varies and depends on whether long-term organ damage has occurred and the underlying disease process.
Many diseases associated with hypercalcemia are curable or manageable with long-term therapies.
TX at a glance
Treat underlying condition, meanwhile:• 0.9% sodium chloride or lactated Ringer's solution for volume expansion (100-125 mg/kg/day IV)• After rehydration: Furosemide- Intermittent pulse therapy-2-4 mg/kg Q 8-12 H IV, SC, PO- Continuous rate infusion-0.66 mg/kg loading dose; then 0.66 mg/kg/hr (~ 5-6 mg/kg Q 8 H)• For severely compromised patients Sodium bicarbonate-1 mEq/kg IV slow bolus• Pamidronate- For vitamin D toxicosis in dogs-1.3-2.0 mg/kg IV over 20 min or 2 hr- In cats-1.0-1.5 mg/kg IV over 2 hr• Glucocorticoid- Prednisolone-1.0-2.2 mg/kg Q 12 H IV, SC, PO- Dexamethasone-0.1-0.22 mg/kg Q 12 H IV, SC, PO• Calcitonin-4-6 IU/kg SC Q 8-12 H