Top 5 Feline Oral Health Concerns
Jeanne R. Perrone, CVT, VTS (Dentistry)

Both dogs and cats suffer from dental disease, but following are 5 oral health concerns more commonly diagnosed in cats.
1. Gingivostomatitis (Caudal Stomatitis)
Stomatitis is defined as an inflammation of the mucous membranes anywhere in the oral cavity.1 This inflammation is more severe than gingivitis or periodontitis because it can extend into the submucosal tissues.
Gingivostomatitis–chronic active inflammation of the mucosa and submucosa–presents with erythematous, ulcerative and/or proliferative lesions commonly found on the gingiva, buccal mucosa, lips, palatal glossal folds, lateral pharyngeal walls, and lateral aspects of the tongue.2-4 (See Figure 1.) No sex, age, or breed predilection exists. The median age of patients with this disease is 7 years.2

Gingivostomatitis showing the extent of oral inflammation. All photos courtesy of the author unless noted otherwise.
The cause is currently unknown, but bacterial, viral, and immunological causes (eg, plaque bacteria, calicivirus, FHV-1, coronavirus, Bartonella henselae, FeLV, FIV, immune reaction) are being investigated.2-4 The most common signs in cats with this disease include halitosis, blood-tinged saliva, ptyalism, dysphagia, difficulty opening the mouth, and weight loss. These cats also become less active, show reluctance to groom themselves, and may become aggressive.2 Caution must be taken when examining these patients’ mouths because they are in pain.
Treatment is a combination of medical and surgical therapy2-4 aimed at controlling the disease. Relapses may occur. Medical therapy may include antibiotics, corticosteroids, pain medications, immunostimulants, and immunosuppressants.2,3 Extracting the teeth in the inflamed areas has shown the best outcome.5 In general, 60% of cases that have surgical intervention will have complete resolution, 20% will have minimal inflammation, 13% will have partial improvement but require continued medical therapy, and 7% will show no improvement.2
2. Juvenile Hyperplastic Gingivitis/Periodontitis
Some form of periodontal disease, the most common inflammatory disease in cats, affects 85% to 95% of cats over age 2, especially if their teeth are not cleaned professionally or home care is not performed regularly.2 One form is juvenile hyperplastic gingivitis/periodontitis, which occurs soon after permanent tooth eruption. This condition is confined to the gingiva, which can become overgrown or hyperplastic.
Significant inflammation begins during eruption of the permanent teeth. The hyperplastic tissue bleeds during mastication, which may make eating difficult and cause the patient pain. The cause is unknown. Susceptibility tends to disappear at about age 2 with consistent professional cleanings that may or may not include hyperplastic tissue removal and at-home care.6 The gold standard for at-home management is brushing because the abrasion of the brush disrupts the plaque bacteria. If the pet is uncomfortable with brushing, oral rinses containing chlorhexidene, along with plaque-controlling diets and treats, can be used.6
Untreated, the disease may progress to juvenile onset periodontitis, in which plaque and calculus form more rapidly and may result in significant gingival recession, furcation exposure, bone loss, and periodontal pocket formation. (See Figure 2.) Teeth that lose more than 50% support should be extracted.
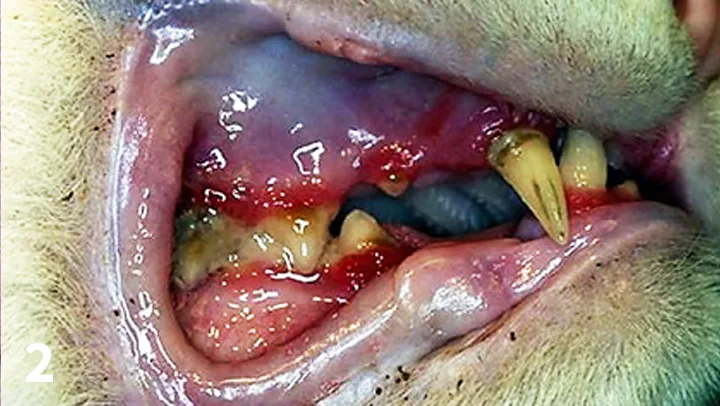
Feline juvenile periodontitis
3. Squamous Cell Carcinoma
These tumors are the most common oral malignancy in cats.7 The lesions are pink, firm, and irregular and usually located in the premolar/molar region in the maxilla, the premolar area in the mandible, and sublingually.7 (See Figure 3.) They are locally aggressive and can metastasize to regional lymph nodes and lungs. Biopsy is crucial for diagnosis, along with aspiration of the affected regional lymph nodes for staging. Therapies include surgical resection, chemotherapy, and palliative radiation. Maxillary and sublingual lesions respond poorly to therapy and have a poor prognosis.7. Mandibular lesions have a better prognosis if caught early when they can be surgically excised with wide margins.7

Squamous cell carcinoma involving the right mandible (arrow)
Patients that undergo surgical excision have a median survival period of one year that may be extended by adjuvant radiation therapy. The median survival period for palliative radiation is 2 to 4 months, which may be extended to 10 months if remission occurs. Sublingual tumors have a grave prognosis with any therapy because most are diagnosed at an advanced stage and inoperable.8
4. Tooth Fracture
Tooth fracture does occur in cats, which have a thinner layer of tooth enamel than dogs.9 Beneath the enamel is a layer of dentin, which is softer, porous, and made up of microscopic tubules that run to the pulp and, when exposed, makes the tooth sensitive. (See Figure 4) Damage to the enamel exposing the dentin is called an uncomplicated crown fracture, which requires treatment because bacteria can enter the bloodstream indirectly through the dentinal tubules. Because the layer of dentin is narrowed compared with that of dogs, the pulp is considered contaminated and extraction or endodontic therapy (ie, root canal therapy) is recommended.9

Fractured right maxillary canine tooth (arrow)
For root canal therapy to be an option, dental radiographs are necessary to rule out open apices (ie, unclosed root tips) that may be seen in a patient younger than a year. If the fracture occurred before the root apex closed, advanced periodontal disease causing major loss of the periodontal support structures (ie, gingiva, periodontal ligament, alveolar bone) or tooth resorption may be seen.9 Root canal therapy involves removing the pulp of the affected tooth, disinfecting the pulp chamber and lining it with a sealer to prevent access to the dentinal tubules, and filling the chamber with a material to remove the dead space, thus restoring the crown of the tooth. Untreated fractured teeth can lead to pulpitis and pulpal necrosis.9,10 Patients requiring root canal therapy should be referred to a veterinary dental specialist. (Under References, see Resources)
5. Tooth Resorption
Tooth resorption is a form of external resorption. Resorption is the loss of hard tissues caused by cells called odontoclasts; external resorptions starts in the root’s cementum layer and can extend into the dentin. Previously called cervical neck lesions, feline caries, and feline odontoclastic resorptive lesions (FORLs), tooth resorption affects 25% to 75% of the cat population over age 2.11 The odontoclasts, which are derived from hematopoietic stem cells, migrate from the blood cells of the periodontal ligament space toward the external root surface and start destroying the dental hard tissue.11 (See Figures 5-7.)
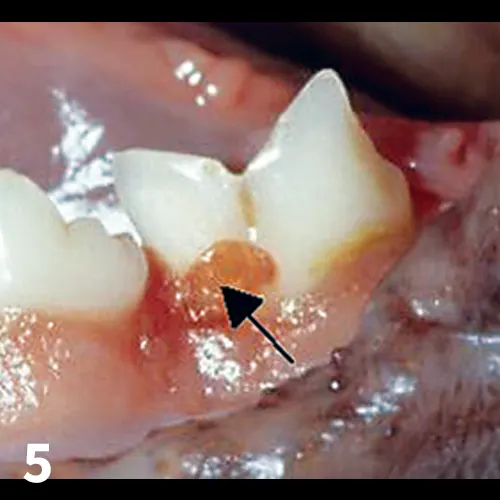
FIGURE 5
Tooth resorption: Note the granulation tissue growing into the enamel defect (arrow)
Three types of tooth resorption, which can only be diagnosed with dental radiographs, are seen. With Type 1, the periodontal ligament and the root remain normal, but there is destruction of the dental hard tissue. (See Figure 8.) With Type 2, the periodontal ligament and roots become indistinct as bone replaces them; with Type 2 lesions, it is evident that while resorption is destroying dental hard tissue, osteoblasts are infiltrating the affected area. Over time, the root contour becomesmore irregular and bone completely replaces the root.12 (See Figure 9.) Teeth can be affected by both Type 1 and Type 2 resorption, which is known as Type 3. (See Figure 10.) The cause of tooth resorption is unknown, although links have been made to periodontal disease, mechanical trauma, immunosuppressive viruses, and increased vitamin A and D intake.11
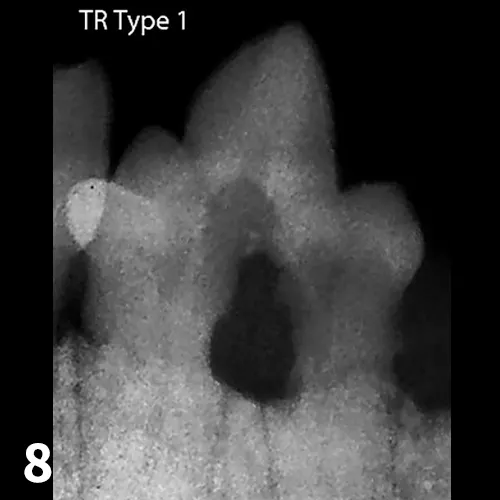
FIGURE 8
Radiograph of tooth resorption Type 1: Note the hard tissue damage at the gumline even though the tooth roots look normal.
Figures 8, 9, and 10 courtesy of AVDC Nomenclature “Types of Resorption Based on Radiographic Appearance.” http://www.advc.org/nomenclature.html#resorption
Diagnosis is made from a visual oral examination using a dental explorer and dental radiographs. (Under References, see Resources) Teeth with any normal structure must be fully extracted; however, if radiographs show the tooth structures have been turned into bone, extraction is not possible and a crown amputation can be performed to the level where recognizable tooth structure does not exist.1 Crown amputation can only be performed on teeth that radiographs confirm as Type 2 and that show no periapical or periodontal bone loss. Crown amputation should not be performed on teeth with Type 1 lesions because those roots are normal and healthy. Crown amputation should also not be performed where stomatitis is present.
Conclusion
Feline oral health problems require a thorough patient history, complete oral examination, and a full diagnostic workup that includes radiographs. Veterinary professionals should always keep current with the treatment options and/or resources to provide the best outcomes for these patients.
This article originally appeared in the January/February 2016 issue of Veterinary Team Brief.