Gallbladder Mucocele in Dogs
Marcella D. Ridgway, VMD, MS, DACVIM (SAIM), University of Illinois
Thomas K. Graves, DVM, MS, PhD, DACVIM, University of Illinois
PROFILE
Definition
Gallbladder mucocele (GBM), a noninflammatory condition of the gallbladder characterized by abnormal accumulation of mucus, forms a gelatinous accretion in the lumen of the gallbladder.
Systems
The gallbladder is the principal organ affected, but inspissated bile may extend into the cystic duct and biliary tree, which can cause obstruction.
Liver disease is identified in ~50% of dogs with GBM.
This may be unrelated to GBM, or the liver may be injured by retained bile acids caused by GBM-related biliary obstruction.
Genetic Implications
Increased occurrence in certain breeds suggests a possible genetic component.
A mutation in the canine ABCB4 gene, which codes for a phospholipid translocator expressed on hepatocyte canalicular membranes, has been associated with GBM in Shetland sheepdogs and other breeds.1
Predisposition to GBM may be secondary to other heritable problems (eg, dyslipidemia, gallbladder dysmotility).
Incidence/Prevalence
Frequency of diagnosis is increasing, possibly because of increased use of ultrasonography.
Geographic Distribution
No regional or seasonal variation of GBM occurrence is recognized.
Signalment
Principally a disease of dogs but has been described in cats and ferrets.2,3
Mean age in dogs: 10 years (range, 3–17 years).4,5
Usually occurs in small to medium-sized dogs, although larger breeds can be affected; no sex predilection.
Shetland sheepdogs4,6-8 and cocker spaniels5,6,9 seem to be overrepresented.
Miniature schnauzers may be predisposed.8
Causes
Underlying cause unknown.
In humans, mucoceles are secondary to obstruction of gallbladder outflow; however, in dogs, experimentally induced biliary obstruction does not result in development of GBM.
Gallbladder dyskinesia is a possible factor.8
Presence of mucosal hyperplasia is a consistent feature but a cause-and-effect relationship has not been established.
Cholecystitis does not appear to be an inciting factor.
Risk Factors
Hypothyroidism, hypercortisolism, diabetes mellitus, pancreatitis, and primary hepatic disease have been proposed to be risk factors.
Age- and breed-matched case-control study reported that the odds of GBM in dogs with hypercortisolism was 29 times greater than that in other dogs.4
GBM is more common in dogs with familial hyperlipidemia.
Increased biliary cholesterol concentration produces more viscous bile and may also increase mucin secretion, further increasing bile viscosity and predisposing to GBM formation.
Pathophysiology
GBM may result from dysfunction of mucus-secreting cells in the gallbladder mucosa.
Gallbladder hypomotility and resultant biliary stasis may also underly this condition.
Progressive accumulation of mucus may cause progressive increases in intraluminal pressure, pressure necrosis of the gallbladder wall, gallbladder rupture, and bile peritonitis.
Signs
Dogs with GBM can exhibit inappetence, vomiting, lethargy, abdominal pain, diarrhea, or icterus.
In >20% of affected dogs, GBM is identified as an incidental finding during abdominal ultrasonography.5
In the single reported case of feline GBM, the presenting signs were weight loss, anorexia, and icterus.
History
In dogs, clinical signs are typically present for a few days to 3 weeks (mean, 5–8 days).
Some dogs have a history of polyuria and polydipsia, likely due to concurrent disease (eg, endocrinopathy, renal disease).
Physical Examination
Some dogs may be asymptomatic at physical examination.
Common findings include hepatomegaly, abdominal pain, icterus, and fever.
Abdominal distention and ascites secondary to bile peritonitis are less frequent findings.
Degree of pain varies from absent to marked.
Diagnosis
Definitive Diagnosis
Diagnosis is confirmed by ultrasonography or surgery.
Immobile echogenic material can be visualized in the gallbladder lumen, often with a characteristic finely striated or stellate (kiwi-fruit) appearance.
Differential Diagnosis
Pancreatitis, cholecystitis, biliary rupture, neoplastic or inflammatory liver disease, cholelithiasis, biliary parasites, pancreatic or biliary neoplasia, and bile duct stricture.
Laboratory Findings
No biochemical or hematologic parameter has been found to be predictive of disease severity or outcome.
Most affected dogs have increased liver enzyme activities and hyperbilirubinemia.
Leukocytosis is seen in about half of affected dogs.
Increased serum urea nitrogen and phosphorus concentrations have been associated with higher mortality in dogs undergoing biliary surgery.10
Hypokalemia was found to be a negative prognostic indicator in Shetland sheepdogs.8
Anemia and hypoalbuminemia have been reported.
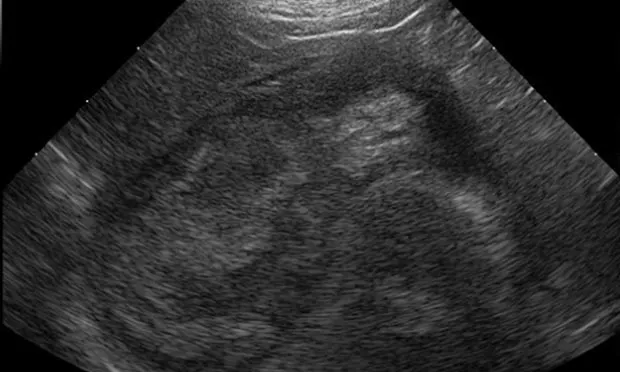
In this ultrasound, the gallbladder contents show a broad hypoechoic region at the periphery that corresponds to the mucosal layer. The central echogenic bile forms a stellate pattern with a distinct border between the hypoechoic and hyperechoic regions. The gallbladder contents were immobile when the patient was repositioned.
Imaging
Radiography
Abdominal radiography is rarely helpful in establishing a diagnosis.
Occasionally, a distended gallbladder may produce a mass-like effect in the right cranioventral abdomen.
Ultrasonography
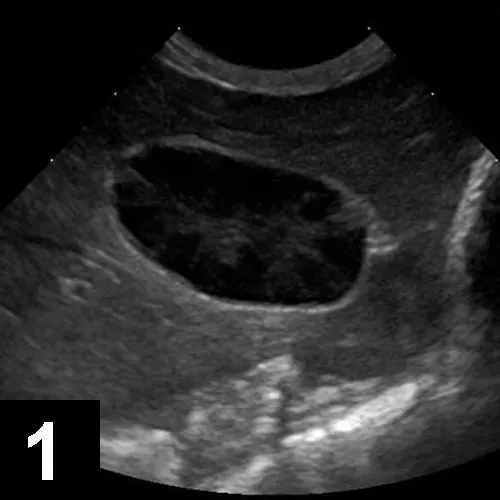
Abdominal ultrasonography is a sensitive and definitive test for GBM (See Figure 1)
In this ultrasound, the gallbladder contents show a narrow hypoechoic region at the periphery with central heterogeneous material filling most of the gallbladder lumen. The irregular hypoechoic areas within the heterogeneous material correspond to areas within the bile accretion with a higher mucus content admixed with areas of echogenic bile. The gallbladder contents were immobile when the patient was repositioned.

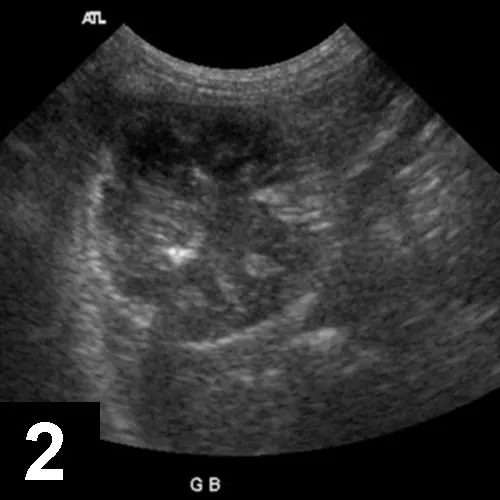
Ultrasonographic appearance of a gallbladder mucocele showing a finely striated bile pattern in the gallbladder periphery and poorly echogenic bile centrally.
Key findings
Gallbladder enlargement.
Immobile echogenic bile on ballottement or repositioning of patient.
Variable findings
Kiwi-fruit appearance.
Thickened gallbladder wall (variable and nonspecific).
Bile duct dilation.
Heterogeneous liver parenchyma.
Findings consistent with pancreatitis.
Echogenic free abdominal fluid.
Mucocele extruded from gallbladder may be visualized in different location.
Other Diagnostics
Abdominocentesis, fluid analysis, and culture for bile peritonitis may be beneficial.
Canine pancreas-specific lipase testing should be conducted for concurrent pancreatitis.
Aerobic and anaerobic culture of bile collected via percutaneous gallbladder centesis or intraoperatively.
Because loss of gallbladder wall integrity is associated with GBM, percutaneous gallbladder aspiration should be undertaken with caution and may not yield adequate samples because of the viscosity of luminal content.
Ultrasonography of gallbladder emptying following ceruletide-induced gallbladder contraction can assess gallbladder motility.
Treatment
Inpatient or Outpatient
Inpatient
Clinically ill dogs should be hospitalized for stabilization, correction of dehydration and electrolyte imbalances, control of vomiting, and management of concurrent peritonitis or pancreatitis.
If surgery is performed, postsurgical hospitalization is 1–7 days (mean, 3.5 days).
Outpatient
Medical treatment is usually administered on an outpatient basis unless initial stabilization with fluids, antiemetics, and analgesics is needed.
Medical
Medical management may be appropriate for asymptomatic or mildly affected patients with no indication of gallbladder rupture or evidence of cholangitis.
Includes choleretics (see Medications), fat-restricted diet (if hyperlipidemic), and monitoring via ultrasonography.
Antibiotics commonly administered because of concerns that biliary stasis could predispose patient to secondary enteric bacterial infection should the gallbladder rupture and lead to septic peritonitis.
Hepatoprotectants such as S-adenosylmethionine (SAMe) are often administered; bile stasis can lead to hepatic injury, and concurrent inflammatory hepatic disease is prevalent.
Patients must be closely monitored for gallbladder rupture.
In reports of medically managed dogs monitored via ultrasonography, GBM often resolved in 2–6 months.
Postmortem Findings
Distended or ruptured gallbladder
Thickened gallbladder wall
Inability to manually express gallbladder
Gelatinous material or semisolid mass-like cast composed of mucus and inspissated bile filling gallbladder lumen
Viscous outer mucosal layer with central dark green gritty material
Congealed mucus and bile in cystic duct and bile duct
Bile peritonitis
Enlarged, mottled liver
Cystic mucinous hyperplasia on histopathology
Concurrent hepatitis or other hepatopathy
Surgical
Cholecystectomy is the surgical treatment of choice.
In virtually all GBM patients, the gallbladder is diseased, with 80% showing microscopic evidence of rupture or gallbladder wall necrosis.
Cholecystectomy is preferable to biliary diversion techniques, and concurrent liver biopsy is recommended.
Patients with gallbladder rupture should be treated as surgical emergencies because of the risk for septic bile peritonitis.
GBM is associated with high perioperative mortality.6,7,10,11
Postoperative complications include bile peritonitis, pulmonary thromboembolism, pneumonia, pancreatitis, sepsis, surgical dehiscence, disseminated intravascular coagulation, and cardiac arrest.
Bile peritonitis is common,6,9-11 with overt gallbladder rupture in 40%–60% of surgical cases.
Perioperative pancreatitis is common and may complicate postoperative recovery but is not associated with increased risk for perioperative death.
Nutritional Aspects
Dogs with hyperlipidemia should be maintained on a fat-restricted diet.
Activity
Activity should be restricted postoperatively as appropriate for patients recovering from abdominal surgery.
Client Education
Owners should be advised that patients treated medically may acutely decompensate because of gallbladder rupture, extrahepatic biliary obstruction, or sepsis.
GBM rarely recurs.
Ancillary Treatment
Fluid therapy to correct fluid and electrolyte abnormalities, pain management, antiemetics, and treatment for concurrent disease may be necessary.
Medications
Choleretics
Ursodiol (15 mg/kg PO q24h or 5–7.5 mg/kg q12h).
Hepatoprotectant.
Promotes secretion of thinner bile.
Should be administered with food.
Contraindicated in dogs with biliary obstruction.
May cause anorexia, vomiting, or diarrhea.
Other Hepatoprotectants
SAMe (20 mg/kg PO q24h).
Antioxidant.
Administer at least 1 hour before feeding; absorption is markedly decreased when given with food.
Store in airtight moisture-resistant container at room temperature.
Potential for additive serotonergic effects when used with tramadol, amitriptyline, clomipramine, monoamine oxidase inhibitors, or serotonin reuptake inhibitors should be monitored.
May cause anorexia, vomiting, or diarrhea.
Antibiotic Selection
Anaerobes and gram-negative aerobes
Ampicillin (20–30 mg/kg PO q8h or 10 mg/kg IV q6h)
Amoxicillin (20 mg/kg PO q12h)
Amoxicillin–clavulanic acid (14 mg/kg PO q12h)
Aerobes, gram-negative and gram-positive cocci and bacilli
Enrofloxacin (2.5–5 mg/kg PO, IM q12h)
Anaerobes
Metronidazole (10–15 mg/kg PO, IV q8–12h); may cause neurotoxicity at acute high or chronic moderate-to-high doses.
Gram-positive anaerobes
Cefazolin (10–30 mg/kg IV, IM q8h for 7 days)
Antibiotics
GBM is usually not associated with bacterial infection, but aerobic bacterial infection has been seen.
Indicated for dogs with positive culture results obtained from gallbladder aspirate or surgical sample.
Antibiotics should be administered for 4–6 weeks postoperatively or for 6–8 weeks with medical management in dogs with positive culture results for bacteria.
Those that are well-distributed in bile should be chosen.
Follow-Up
Monitoring
GBM is associated with significant perioperative complications, but long-term outlook is good for dogs surviving to hospital discharge.
Complications tend to occur immediately but have been reported up to 3 weeks after surgery.
Clinicopathologic abnormalities improve or resolve within 2 weeks–3 months.
In patients managed medically, gallbladder rupture appears to be infrequent and occurs within 2 weeks of diagnosis.8,12,13
CBC, serum liver enzyme activities, and bilirubin concentration should be monitored q2–4wk until normalized.
Follow-up abdominal ultrasonography should be performed in dogs treated medically.
Prevention
When present, treatment for hyperlipidemia and management of endocrinopathy may be beneficial in preventing GBM.
Future
Dogs should be evaluated at 2 and 4 weeks postoperatively for overall clinical status, serum biochemistry parameters, and abdominal ultrasonography findings.
Complete resolution of clinical signs, normalization of bilirubin concentrations, and improvement in serum liver enzyme activities is expected, but many recovered dogs have persistent increases in liver enzyme activity.
In dogs with bile duct dilation, the common bile duct may remain distended without clinical signs.
For dogs treated medically, follow-up evaluations should be performed q2mo until GBM has resolved.
In General
Relative Cost
Initial diagnostic evaluation $$$
Surgical treatment $$$$$+
Medical treatment and follow-up $$$$
Prognosis
Long-term prognosis is excellent for dogs that survive the perioperative period.
Outcome of limited numbers of dogs treated medically has not been objectively evaluated, but reported cases did well long-term. One death from gallbladder rupture and one GBM recurrence were reported.
Future Considerations
Controlled evaluation of outcomes in dogs treated medically should be undertaken to assess the safety and effectiveness of this alternative to surgical treatment.
Further study of GBM pathogenesis and predisposing factors should be pursued.
Significance of biliary sludge as a possible preliminary stage that should be treated to prevent progression to GBM should be addressed.
GBM = gallbladder mucocele, SAMe = S-adenosylmethionine