Visualizing Feline Skin Fragility Syndrome

FIGURE 1 Thin, friable, wet, tissue paper–like skin secondary to spontaneous hyperadrenocorticism
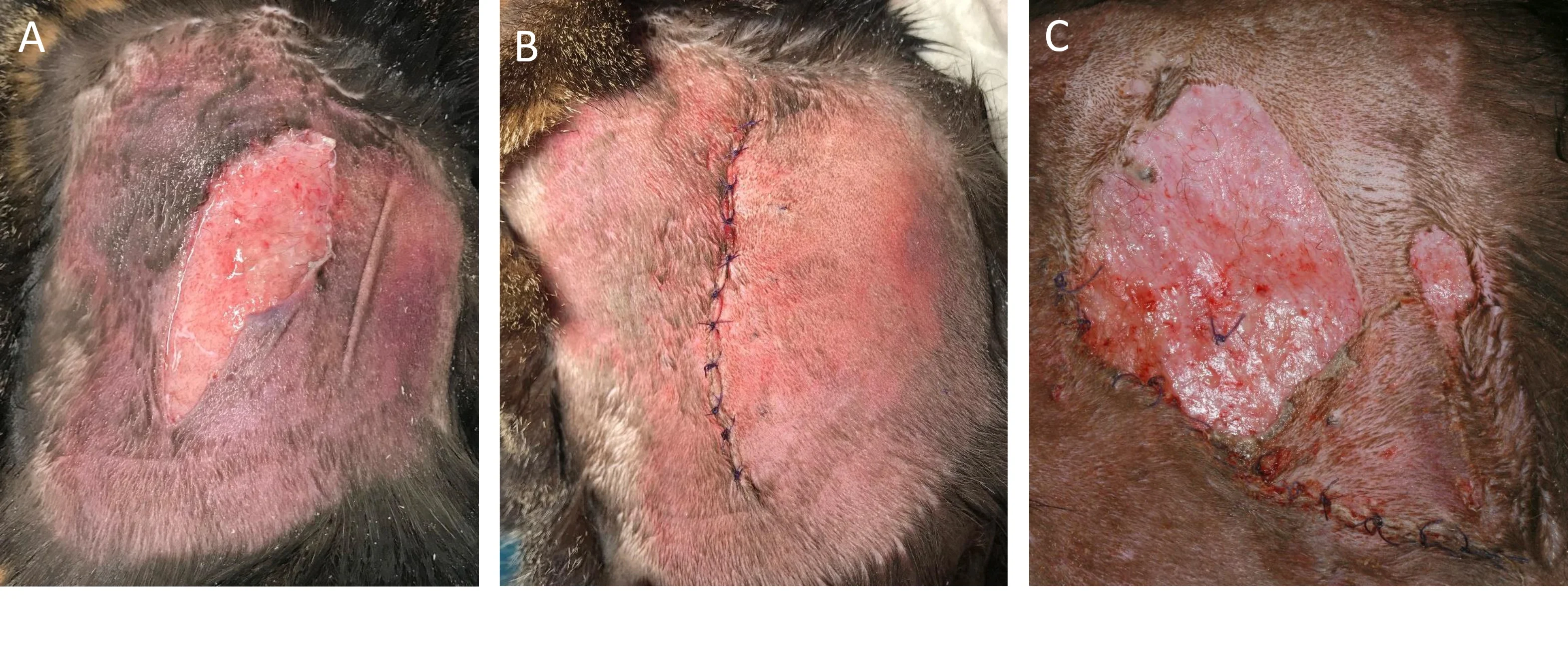
FIGURE 2 Iatrogenic FSFS (A) caused by repeated, overlapping depot methylprednisolone injections. Despite surgical treatment (B) and continued hospitalization, the skin reopened within 1 day following surgery (C).
Understanding Feline Skin Fragility Syndrome
Feline skin fragility syndrome (FSFS) is a rare, acquired disorder characterized by markedly thin skin that easily tears following minimal trauma. FSFS is visually striking and considered a dermatologic emergency. Skin wounds are accompanied by minimal bleeding and are difficult to manage. Concurrent generalized demodicosis (ie, Demodex cati) may be present.
Quality-of-life discussions should be initiated promptly with the pet owner. Hospitalization with immediate administration of analgesia and topical antimicrobial treatment is needed. Extremely careful handling and restraint should be emphasized during hospitalization, investigation, and treatment. Further catastrophic skin trauma may occur with simple coat clipping, wound dressing and redressing, clothing application, claw covering, hair plucking (Demodex spp), phlebotomy, and cystocentesis.
Differential diagnoses include endocrinopathy (most common, ≈50% of cases; spontaneous hyperadrenocorticism ± diabetes mellitus), as well as iatrogenic (topical or systemic glucocorticoid, progestogens, phenytoin), infectious (FIP), inflammatory/infectious (cholangiohepatitis), metabolic (anorexia ± hepatic lipidosis), and neoplastic (cholangiocarcinoma and multicentric lymphoma) causes. Some of these conditions have negative effects on collagen synthesis, which is the proposed mechanism of FSFS.
If thorough assessment of clinical history does not reveal the likely cause, investigation can be initiated with a free-catch urinalysis and cortisol:creatinine ratio measurement using nonabsorbent litter and no patient handling. Additional investigation should be performed with the patient under chemical restraint (IM administration) and may include phlebotomy to collect blood for CBC, serum chemistry profile, and virology (ie, FIP), as well as abdominal ultrasonography. Fluid or tissue sampling during abdominal ultrasonography should be performed via fine-needle aspiration to avoid risk for further skin trauma from more invasive sampling techniques. Esophagostomy tube placement for assisted feeding and medication administration and primary reconstructive surgery with the patient under general anesthesia may also be considered.
Prognosis is grave, but iatrogenic (especially due to topical or oral medications) and anorexia-associated (in cases in which the cause of anorexia can be managed) FSFS are potentially reversible.