Radiography is often recommended prior to ultrasonography for foreign body diagnosis because it is cheaper, is more readily available, provides results that are easier for the general clinician to obtain and interpret, can help provide an accurate diagnosis in most cases, and can provide a global view of the abdominal and regional extra-abdominal structures.1 Some patients, however, require additional diagnostic imaging when a foreign body or obstructive radiographic gas pattern cannot be seen. If available, ultrasonography can eliminate superimposition of abdominal structures and allow more thorough evaluation of a large portion of the GI tract. Ultrasonography can diagnose small intestinal mechanical obstruction with greater accuracy than radiography.1,2
Limitations of Ultrasonography
Ultrasonography and those trained to perform diagnostic ultrasonography are not typically readily available in the general clinic. The accuracy of ultrasonography depends on user skill in interrogating the abdomen; however, with appropriate training, nonradiologists (eg, general clinicians, other specialists, sonographers, licensed veterinary technicians) can identify foreign body obstructions via ultrasonography. Ultrasonography examination takes longer to perform and is more expensive than standard abdominal radiography. Although ultrasonography can help evaluate soft tissues and fluid in the body, it cannot help with visualization beyond gas or bone interfaces due to complete reflection and/or absorption of the ultrasonography beam, especially in the stomach (where gastric foreign bodies and pyloric obstructions are often easier to identify via radiography).
Point-of-Care Ultrasound
In clinics without individuals trained to perform full diagnostic ultrasonography, abdominal point-of-care ultrasound (POCUS) can help assess patients with anorexia, vomiting, and/or acute abdominal pain. Abdominal POCUS can accurately identify free peritoneal effusion and gas, which are common in patients with septic peritonitis, a condition that requires immediate stabilization and surgical intervention regardless of the underlying cause.3-5 The role of abdominal POCUS in diagnosing small intestinal obstructions is unclear in veterinary medicine and still emerging in human medicine.6-8 In humans, POCUS is less accurate than diagnostic ultrasonography, with a reasonable sensitivity and specificity that is highly dependent on user skill and experience level.6-8 As of the time of writing, abdominal POCUS cannot be recommended in place of diagnostic ultrasonography if available.
Ultrasonographic Appearance of Foreign Bodies
The majority of GI foreign bodies are denser than surrounding soft tissues and fluid. Most of the ultrasonography beam is reflected when there is a sudden change in tissue density (more accurately, acoustic impedance), and further echoes deep to that surface are not produced. The resultant image is a bright hyperechoic line that contours to the shape of the foreign body (eg, plastic toys, rubber balls, cloth, bones, metal), with variable distal acoustic shadowing (Figure 1).9-12 Foreign bodies filled with gas have a similar appearing hyperechoic surface but cause a reverberation artifact (ie, dirty shadow). The entire foreign body will be visible if it is hollow and filled with fluid or has a density similar to soft tissue. Locating foreign bodies can be challenging when only the surface is visualized, but ultrasonography can help detect other changes associated with pyloric outflow, small intestinal mechanical, and linear foreign body obstructions.
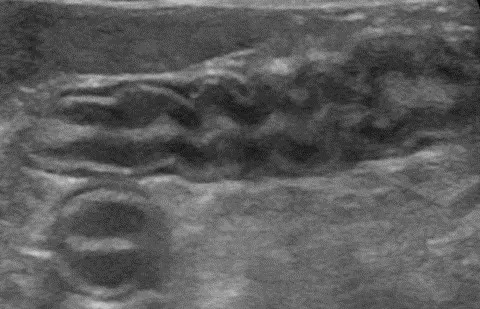
Abdominal ultrasound of a 6-year-old neutered male crossbreed dog with a surgically confirmed foreign body (cloth) in the duodenum. The cloth is seen as a hyperechoic curvilinear structure (arrow) that causes a distal acoustic shadow (asterisk).
Pyloric Outflow Obstructions
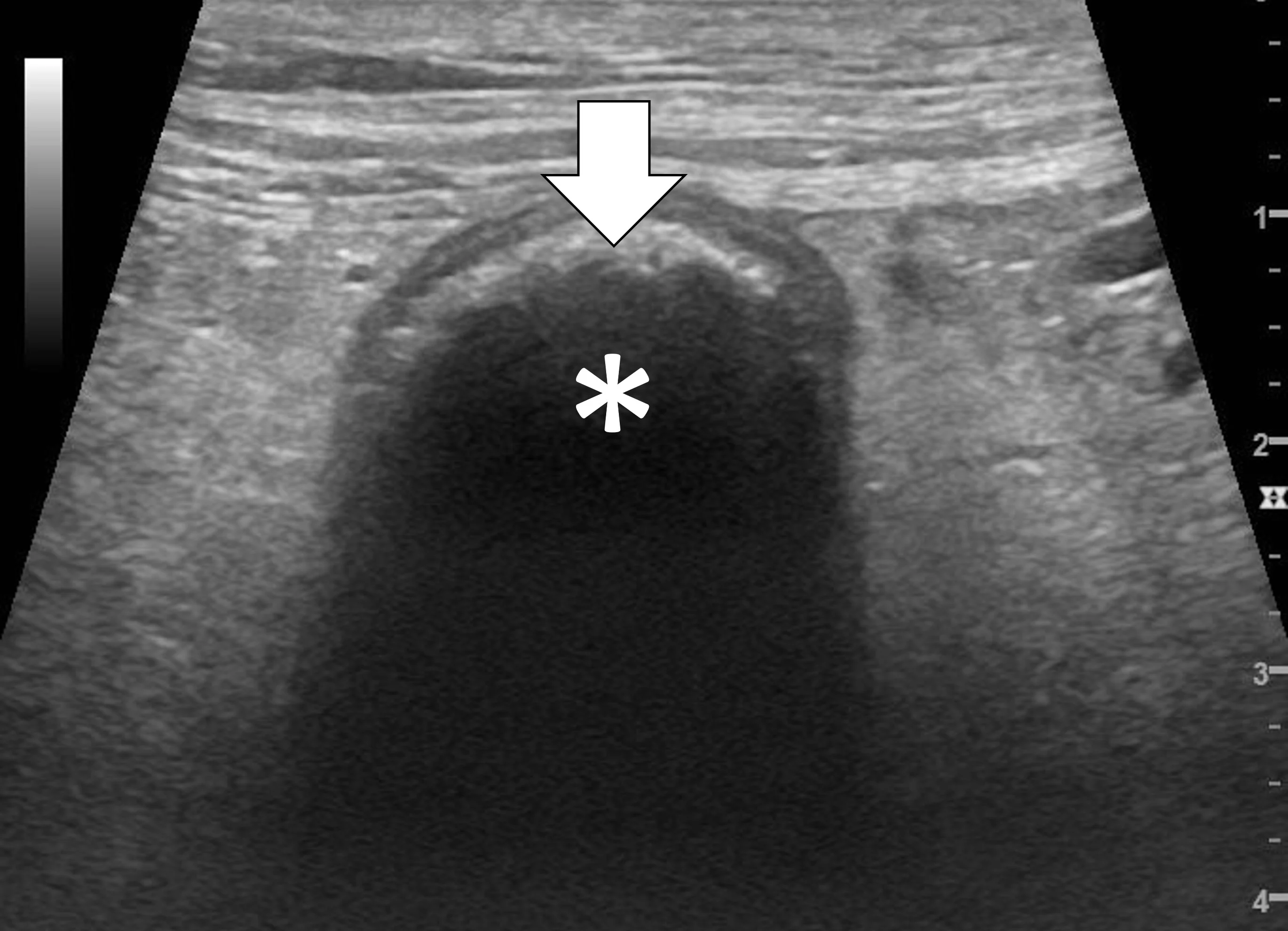
Pyloric outflow obstructions occur when a foreign body lodges in the pyloric outflow tract or the proximal duodenum and can cause variable gastric distention depending on the length of time the obstruction has occurred and whether the patient has recently vomited (Figure 2). Diagnosis of this type of obstruction via ultrasonography requires identification of an intraluminal structure that is causing gastric or proximal duodenal dilation orad to the foreign body.9-12 Foreign bodies are easier to see when surrounded by fluid. Although exceptions are possible, acute complete obstructions typically cause mild to moderate gas dilation, and chronic partial obstructions can cause more moderate to severe dilation, predominately with fluid.
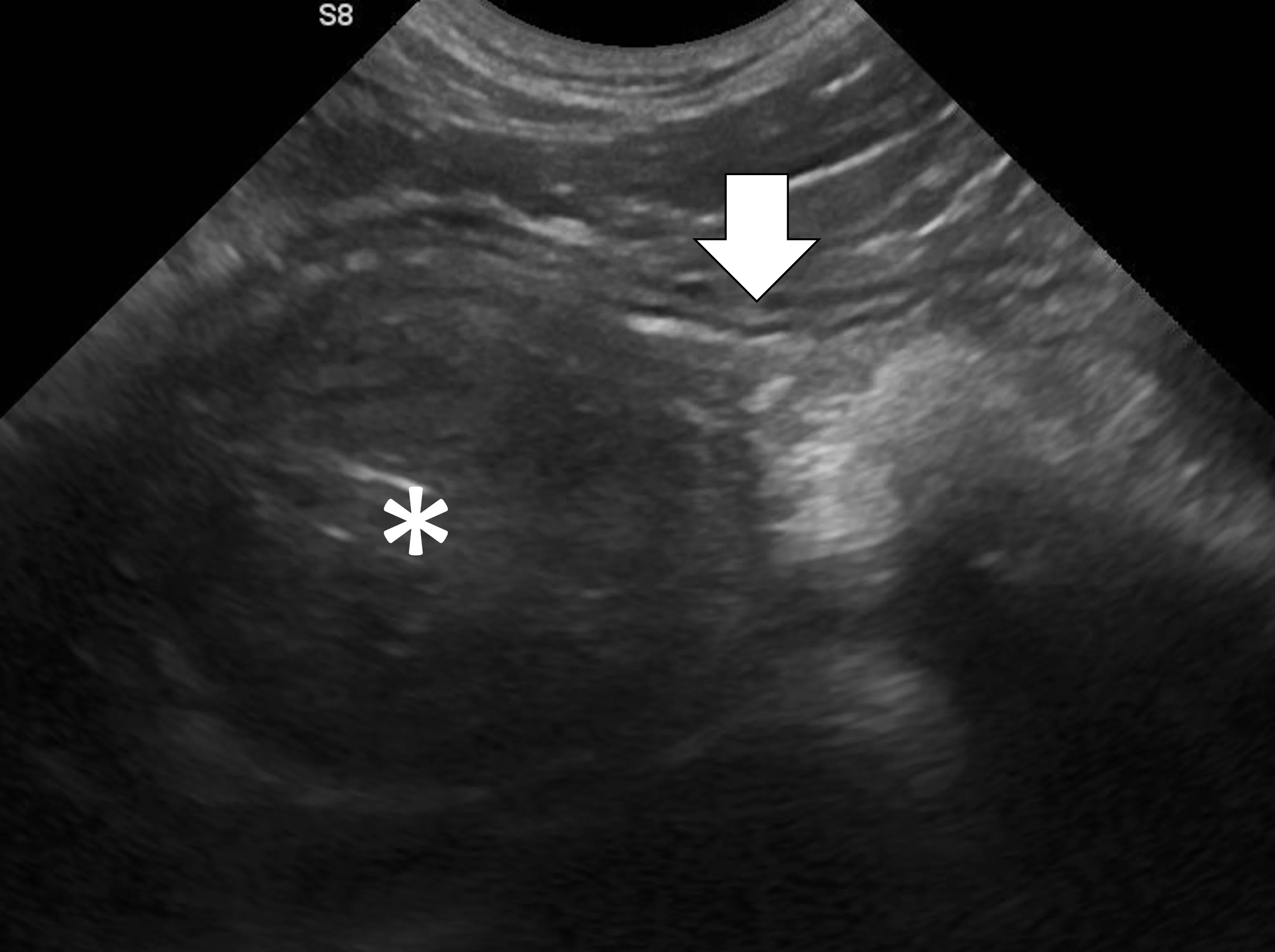
FIGURE 2A
Abdominal ultrasound of a 3-year-old neutered male crossbreed dog with a surgically confirmed mechanical pyloric outflow obstruction. A homogeneously hypoechoic potato (asterisk) is present in the pylorus and completely visible due to its similar acoustic impedance as the surrounding soft tissues. There is transition from gas in the gastric lumen to the foreign body (white arrow). The remainder of the gastric lumen (pound sign) is not visible due to gas (black arrows) causing a hyperechoic surface with reverberation artifact.
Only the gastric wall located in the near field is visible if the stomach is filled with gas. The stomach may need to be evaluated from multiple angles, including subxiphoid, subchondral, right intercostal, and left intercostal. The pylorus shifts craniodorsally and is more difficult to see when the stomach enlarges and the patient is in dorsal recumbency. In these situations, the right intercostal approach can make finding the pylorus and proximal duodenum easier. Evaluating the stomach with the patient in different positions (eg, dorsal recumbency, lateral recumbency, standing) changes the distribution of fluid and gas and may aid in foreign body detection. Gas within the lumen of the stomach masks intraluminal structures; therefore, ultrasonography cannot rule out a gastric foreign body in a gas-dilated stomach.
Small Intestinal Mechanical Obstructions
Small intestinal mechanical obstructions occur when a foreign body blocks the lumen of any segment of the small bowel, causing segmental dilation located orad to the foreign body (Figure 3).9-12 As the small bowel increases in size, it crowds the peritoneal cavity and begins stacking on itself with sharp, hairpin turns.9-12 Dilated portions of the small bowel usually contain a mixture of fluid and gas. One study demonstrated that a serosal-to-serosal jejunal diameter of >1.5 cm helped discern dogs with and without mechanical obstruction.1 Dilated bowel can often be followed to the site of obstruction, where it immediately normalizes aborad to the foreign body. In some patients, the foreign body may not be visualized if located deep to more superficially located gas-dilated intestines. In patients scanned in dorsal recumbency, gravity may cause heavier foreign bodies to settle deep in the abdomen. If jejunal dilation >1.5 cm is present but the site of obstruction is not initially seen, the patient may be shifted into right and then left lateral recumbency and the midabdomen reinterrogated. In addition, one study suggested that a foreign body may be palpated in a majority of cases13; physical examination may therefore expedite ultrasonography. If the foreign body can be manually held or trapped against the body wall, ultrasonography can be performed on that location; however, identifying the site of obstruction is not always necessary if segmental dilation is present and the clinical picture supports a diagnosis of mechanical obstruction.
Abdominal ultrasound of a 9-month-old spayed Australian cattle dog with a surgically confirmed small intestinal mechanical obstruction. There is moderate small intestinal dilation (asterisk) with hyperechoic fluid, ingesta, and gas measuring 2.1 cm in diameter at the level of the white calipers oral to a pecan foreign body (pound sign) that is visible as a hyperechoic surface with distal acoustic shadowing. The small intestine is normal and not dilated immediately aboral to the foreign body (arrow), with a small volume of intraluminal gas causing reverberation artifact.
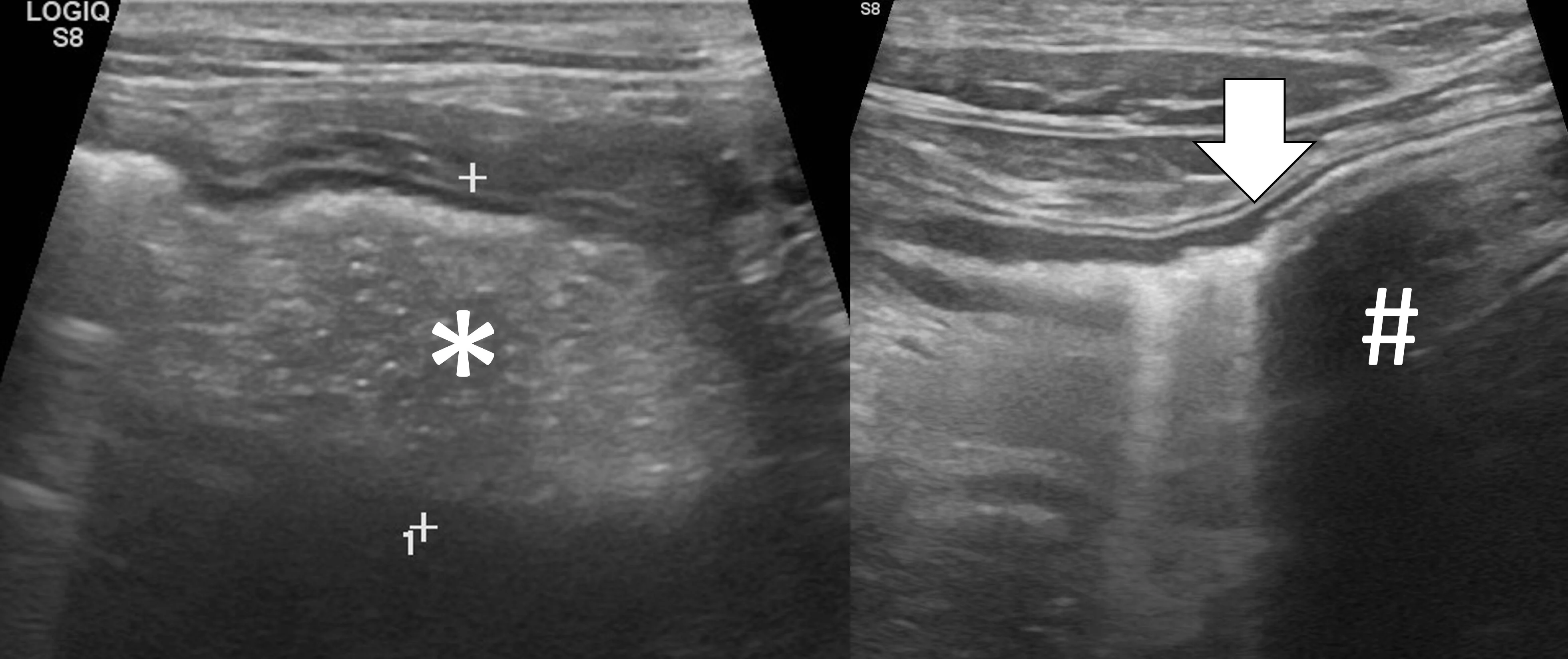
Linear Foreign Body Obstructions
Linear foreign body obstructions occur when an object (eg, string, cloth) becomes stuck orally but extends aborally through the intestinal tract. Peristaltic contractions typically cause the small intestine to travel orally, eventually bunching. As a result, ultrasonographic findings include intestinal bunching (ie, plication) with or without a hyperechoic linear structure coursing through the lumen of the affected bowel (Figure 4).9-12 In some cases, trapped gas can cause a line that can be mistaken for the linear foreign body. Plication should not be confused with normal peristalsis or corrugation (Figure 5). With corrugation, the serosal margin is normal, and the mucosa and submucosa are undulant; with plication, the serosal margin is affected.14 In chronic cases, the mesentery surrounding the affected bowel may become hyperechoic, which can help identify the site of obstruction. Sterile inflammation and transudation may then result in focal accumulation of a small volume of free fluid. Mesenteric changes and peritoneal effusion also increase concern for bowel rupture and septic peritonitis. Patients may have concurrent findings of pyloric outflow or small intestinal mechanical obstruction, depending on the size and nature of the ingested cloth or string.
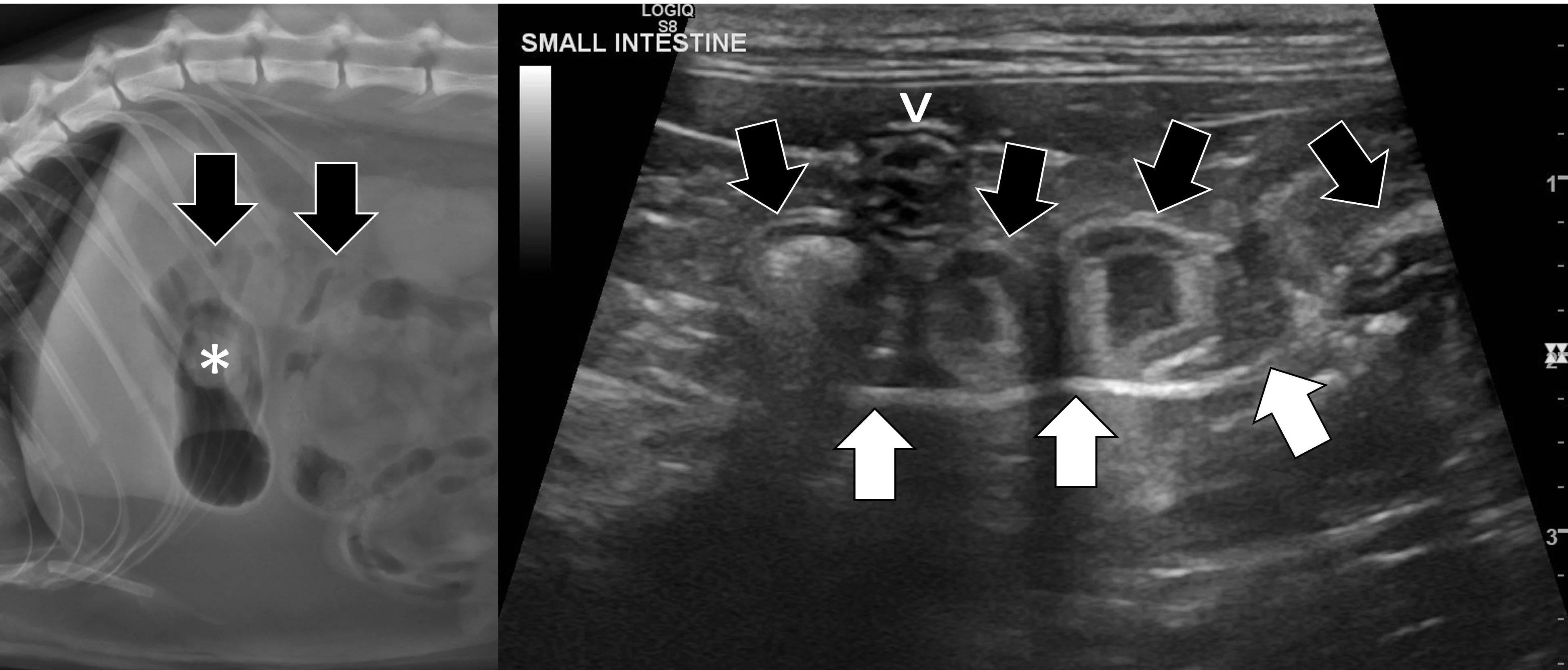
Abdominal ultrasound of an 11-month-old neutered male domestic shorthair cat with a surgically confirmed toy ball connected to a linear foreign body anchored in the pylorus (asterisk). The proximal duodenum is plicated (black arrows) with a hyperechoic linear structure (white arrows) coursing through the center. Normal small intestine can be seen adjacent to the plicated duodenum (caret).
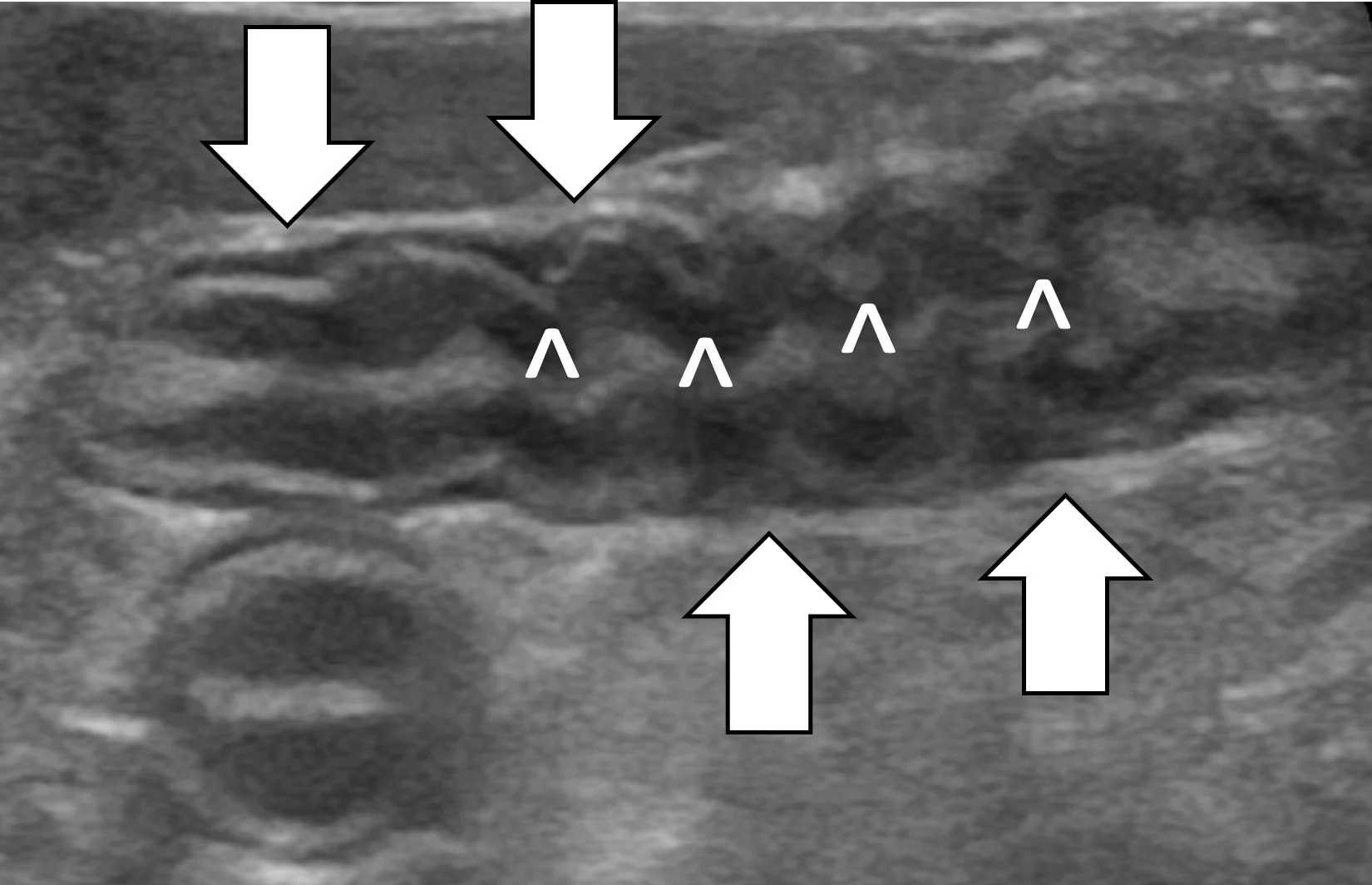
Abdominal ultrasound of an 8-year-old spayed miniature pincher with inflammatory bowel disease and pancreatitis. The mucosal and submucosal layers of a loop of jejunum are undulating (carets), but the serosal margin remains smooth (arrows).
Listen to the Podcast
Dr. Seitz joined the podcast to share his expertise on how to use radiography to the fullest and how to apply point-of-care ultrasound at the general practice level.