Fluid Therapy
Adesola Odunayo, DVM, MS, DACVECC, University of Florida

Fluid therapy is an essential therapeutic component in small animal practice. Normal cellular function can be impaired without water and potentially lead to patient death.1 Intravenous fluids may be prescribed to hospitalized patients to treat hypovolemia, dehydration, electrolyte imbalance, and acid-base abnormalities and to ensure that adequate cellular maintenance requirements are met.2
Fluid Compartments
Understanding the concept of fluid compartments can help the clinician determine the location of the fluid deficit and appropriate treatment. The body weight of nonobese cats and dogs is composed of approximately 60% water.2 Puppies and kittens have higher total body water amount (ie, up to 80% of body weight), as total body water decreases with age.3 In addition, fat has a lower water content; thus, the fluid prescription should be based on estimated lean body weight.4 In adult nonobese cats and dogs, approximately two-thirds of total body water (ie, 66% of total body water or ≈40% of body weight) is in the intracellular space. The remaining one-third (ie, 33% of total body water or ≈20% of body weight) is in the extracellular space; of this extracellular body water, 75% (≈15% of body weight) is in the interstitial space and 25% (≈5% of body weight) is in the intravascular space. Intracellular fluid loss is generally not appreciated on physical examination and typically manifests as hypernatremia. Treatment of intracellular fluid deficit is beyond the scope of this article.
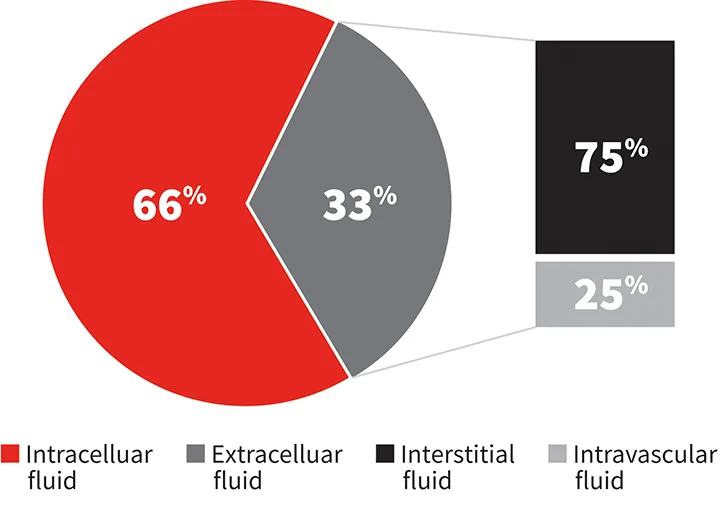
Distribution of total body water in an adult nonobese cat or dog
Intravascular fluid deficit (ie, hypovolemia) leads to inadequate oxygen delivery to the cells (ie, poor perfusion or shock). Untreated intravascular fluid deficit can be life-threatening, as oxygen is important for minute-to-minute cellular function maintenance. Inadequate oxygen delivery can lead to hyperlactatemia through anaerobic glycolysis, cell membrane disruption, cell death, and organ death.5 Physical examination findings of hypovolemia (Table 1) include tachycardia in dogs, bradycardia in cats (and in the terminal stages of shock in dogs), prolonged capillary refill time, pale mucous membranes, weak peripheral pulses, cold extremities, and altered mental state. Patients exhibiting these signs require emergent treatment to rapidly restore oxygen delivery. Common clinical conditions that lead to intravascular fluid loss include hemorrhage secondary to trauma, coagulopathy, neoplasia, gastroenteritis, pancreatitis, and peritonitis.
Table 1: Physical & Laboratory Abnormalities in Patients With Hypovolemia and Dehydration
* Cats tend to demonstrate this triad.
Interstitial fluid deficit (ie, dehydration) is commonly assessed based on a percentage of the estimated interstitial fluid lost (Table 2) and typically does not result in life-threatening abnormalities unless dehydration progresses to approximately 9% or greater. Signs of dehydration that may be identified on physical examination include skin tenting, dry mucous membranes, doughy abdomen, and sunken eyes. The different clinical approaches and urgency for treating poor perfusion and dehydration make differentiating between them vital (Table 1).
Table 2: Physical Examination Findings of Dehydration and Estimate of Fluid Loss Percentage
*Death is imminent.
Fluid Types
A crystalloid is a water-based solution composed of osmotically active small molecules that are permeable to the capillary.6 A significant percentage of crystalloids move into the interstitial and intracellular space within approximately 45 minutes of intravenous administration. Isotonic crystalloids (eg, 0.9% NaCl, lactated Ringer’s solution), which are primarily used for fluid therapy in veterinary medicine, have osmolality similar to plasma and therefore do not cause cellular swelling or shrinkage when administered.6 Hypotonic and hypertonic crystalloids have lower and higher osmolality, respectively, as compared with plasma.
Synthetic colloids (eg, hydroxyethyl starch solutions) are crystalloid-based fluids composed of large molecules that do not cross the capillary membrane. Colloids can be used to treat hypovolemia and/or hypoproteinemia.7-9 Synthetic colloids should be used cautiously in veterinary patients10,11 because of concerns in human patients that acute kidney disease and coagulopathies may develop.
Fluid Prescription
A quick stepwise approach that provides an individualized fluid plan for the patient is needed once it has been determined that fluid therapy may be beneficial. Using a fluid prescription consisting of 3 straightforward steps (vs arbitrarily putting a patient on a 2× maintenance fluid rate) ensures that the patient’s fluid deficit is identified and corrected in a timely manner (see Examples of Individualized Fluid Plans, below). Ongoing fluid losses are not included in this plan but should be replaced in patients with significant ongoing fluid loss (eg, a puppy with parvoviral enteritis with continued vomiting and diarrhea).
Hypovolemia and dehydration can occur independently of each other; therefore, dehydrated patients may not be hypovolemic, and hypovolemic patients may not be dehydrated.
Step 1: Resuscitation
(Identify & Treat Hypovolemia if Present)
Hypovolemia can lead to poor oxygen delivery and should be identified (Table 1) and treated quickly.12 If hypovolemia is suspected or identified, fluids should be administered intravenously or via the intraosseous route.
Fluids administered subcutaneously, in the peritoneal cavity, or through the oral route are not absorbed well because blood flow is diverted to the heart, lungs, and brain in a hypovolemic state. Cats with evidence of hypovolemia should be actively warmed to a body temperature of at least 97°F (36°C) before large volumes of fluids are given.
The shock dose is an estimate of the total blood volume (dogs, 90 mL/kg/hr; cats, 60 mL/kg/hr). It is unlikely that a hypovolemic patient will have lost its entire blood volume; thus, approximately 25% of the fluid prescription (dogs, 20 mL/kg/15 min; cats, 15 mL/kg/15 min13) should be administered using pressure bags, fluid pumps, or a 60-mL syringe. Fluid pumps run at 999 mL/hr and are best used for boluses when the total volume to be infused over 15 minutes is less than 250 mL.
The patient should be re-evaluated after the fluid bolus is given. Additional fluid boluses can be administered (dogs, ≤90 mL/kg/hr; cats, 60 mL/kg/hr) if clinical parameters of hypovolemia have improved but are not yet satisfactory (see Oxygen Delivery Restoration Parameters). Fluid administration can be discontinued when the patient has met the desired criteria, but, because isotonic crystalloids have a short lifespan in the intravascular space, the patient’s vital parameters should be monitored closely.
Synthetic colloids (eg, hydroxyethyl starch solutions; 1-5 mL/kg every 15 minutes) can be used to treat hypovolemia. The author prefers to use the low end of the dose range for cats, whereas dogs tend to tolerate the higher end.
OXYGEN DELIVERY RESTORATION PARAMETERS
Normal heart rate (dogs, 100-140 bpm; cats, >160 bpm)
Pink mucous membranes
Normal capillary refill time (<2 seconds)
Normal peripheral pulses
Improved mentation
Improved blood pressure (100-140 mm Hg systolic)
Improved serum lactate (1-2.5 mmol/L)
Step 2: Rehydration
(Identify & Treat Dehydration if Present)
After hypovolemia (if present) is treated, the patient should be evaluated (Table 1) and treated for dehydration as needed. The fluid deficit in the interstitial space can be determined by multiplying the patient’s body weight by the estimated dehydration percentage (Table 2)1:
Fluid deficit (liters) = weight in kg × % dehydration
The fluid deficit is then replaced over a period of 6 to 24 hours1 using any isotonic crystalloid. The author prefers to replenish the fluid deficit over 6 to 8 hours except in cats and in patients with underlying heart disease, in which the fluid deficit is replaced over 12 to 24 hours.
Step 3: Maintenance
(Provide Cellular Maintenance Requirement)
Cells have a daily water requirement to maintain regular metabolism. Maintenance fluids (dogs, 60 mL/kg/q24h; cats, 45 mL/kg/q24h12) can be provided as part of the fluid plan when a patient is not eating or drinking, in addition to correcting dehydration and restoring perfusion. Multiple units of the maintenance dose (rates 2× or more above the maintenance rate) can be provided to patients that may benefit from diuresis (eg, after exposure to toxins). Isotonic crystalloids are typically used to provide maintenance requirements, but hypotonic crystalloids (eg, 0.45% NaCl) may also be used.
Complications of Fluid Therapy
Like any drug used in clinical medicine, fluids are not benign, and their use can potentially lead to life-threatening complications, including respiratory distress secondary to volume overload, coagulopathies, electrolyte abnormalities, acid-base disturbances, and propagation of inflammation.14 Fluid prescriptions should be individualized and the patient monitored often to detect any adverse effects associated with fluid therapy.
Examples of Individualized Fluid Plans
Example 1
Gerald, a 4-year-old neutered male cat weighing 6.6 lb (3 kg), is presented for vomiting and diarrhea of 3 days’ duration. He was anorexic and lethargic prior to presentation.
On physical examination, Gerald is quiet and has a heart rate of 120 bpm, pale mucous membranes with a capillary refill time of about 2 seconds, weak peripheral pulses, initial blood pressure of 50 mm Hg (systolic), and a body temperature of 94°F (34°C). He is also estimated to be about 6% dehydrated based on skin tenting and dry mucous membranes.
Step 1: Resuscitation
Gerald has signs of hypovolemia (ie, bradycardia, hypotension, hypothermia, weak peripheral pulses, pale mucous membranes) and should be resuscitated immediately to restore oxygen delivery.
A peripheral catheter—or intraosseous catheter if a peripheral catheter is difficult to place—should be used. The medial saphenous veins may be easier to access in hypovolemic cats.
Exogenous heating (eg, forced air warming devices) should be used to raise body temperature to at least 97°F (36°C).
A 45-mL (15-mL/kg) balanced isotonic crystalloid (eg, lactated Ringer’s solution, 0.9% NaCl) should be administered over 15 minutes using a 60-mL syringe or a fluid pump.
Parameters should be reassessed and stopped if the patient has met the end goals (see Oxygen Delivery Restoration Parameters).
As the patient’s body temperature rises, additional fluid boluses can be given, if needed.
Step 2: Rehydration
Gerald responded well to the fluid given during resuscitation. His heart rate is now 200 bpm, blood pressure is 100 mm Hg, and mucous membranes are pink. He still has signs of dehydration based on skin tenting and dry mucous membranes and is estimated at 6% dehydration. This fluid deficit should be replaced using an isotonic crystalloid.
Fluid deficit calculation:
Fluid deficit (liters) = weight in kg (3) × % dehydration (0.06)
Fluid deficit = 3 × 0.06
Fluid deficit = 0.18 L (180 mL)
Timeframe needed to replace the fluid deficit (cats tend to be less fluid tolerant; Gerald’s deficit will be replaced over 12 hours):
180 mL q12h = 15 mL/hr for 12 hours
Step 3: Maintenance
Hourly fluid requirements (ie, maintenance fluids) should be provided to maintain normal cellular activity. Because the patient is not eating or drinking, the maintenance requirement should be provided using an isotonic crystalloid; a hypotonic crystalloid can also be used to provide maintenance requirements.
The maintenance fluid requirement is:
45 mL/kg q24h (45 × 3) = 135 mL/q24h or 6 mL/hr
Overall fluid prescription after treating hypovolemia is:
Fluid deficit (15 mL/hr) + maintenance (6 mL/hr) = 21 mL/hr for the first 12 hours; fluid rate is then reduced to 6 mL/hr (provided there are no ongoing fluid losses)
Example 2
Sasha, a 4-year-old female Dachshund weighing 15.4 lb (7 kg), is presented for evaluation after being hit by a car. Physical examination findings reveal a heart rate of 160 bpm, pale mucous membranes, a capillary refill time of 3 seconds, and weak peripheral pulses. She has a broken left femur and some abrasions associated with the fracture. The remainder of the findings are within normal limits.
Step 1: Resuscitation
Sasha has signs of hypovolemia (ie, poor perfusion) based on tachycardia, prolonged capillary refill time, and weak peripheral pulses.
A large-bore intravenous catheter should be placed and fluid therapy initiated to restore oxygen delivery. An analgesic—ideally opioids—should be administered for fracture-associated pain that may also lead to tachycardia.
A 140-mL isotonic crystalloid bolus should be administered (20 mL/kg) rapidly over 15 minutes. A fluid pump may be used.
Physical examination parameters should be reassessed to ensure end goals (see Oxygen Delivery Restoration Parameters) have been met after providing a fluid bolus. The crystalloid dose may be repeated up to 90 mL/kg/hr.
Step 2: Rehydration
Physical examination findings consistent with dehydration are not found. This step can be skipped.
Step 3: Maintenance
Because Sasha is not likely to begin eating or drinking immediately, she will likely benefit from maintenance fluids.
Maintenance fluid requirement is:
60 mL/kg q24h (60 × 7) = 420 mL q24h or 18 mL/hr
Overall fluid prescription after treating hypovolemia is:
Fluid deficit (0 mL/hr) + maintenance (18 mL/hr) = 18 mL/hr until she starts to eat and drink on her own (provided there are no ongoing fluid losses)