Flail Chest: Diagnosis & Bandaging
Daniel McCarthy, DVM, Coral Springs Animal Hospital, Coral Springs, Florida
Brett Darrow, DVM, University of Tennessee
Karen M. Tobias, DVM, MS, DACVS, University of Tennessee
Hannah Evans, DVM, University of Tennessee
Dottie Williams, DVM, University of Tennessee
Colleen Monahan, DVM, University of Tennessee
Nakeita Fowler GeFellers, DVM, University of Tennessee
Flail chest refers to a freely movable segment of the thoracic wall secondary to fractures of consecutive ribs.
In most cases of flail chest, each affected rib is fractured at multiple sites; however, a flail segment can be present in animals with single fractures on affected ribs or with dislocations or flexible costal cartilage (Figure 1). This may result in respiratory compromise caused by pain, trauma to the lungs, or decreased ventilation. Flail chest is a potential consequence of a traumatic event involving extreme external forces (eg, dog attack, motor vehicle accident trauma).1
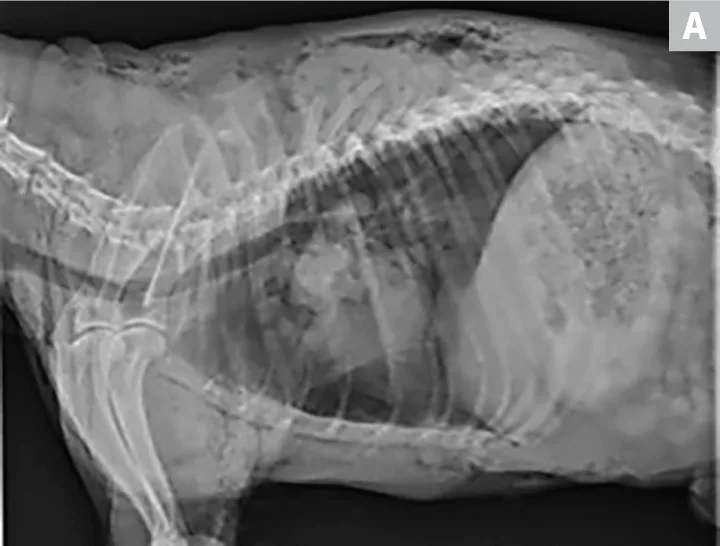

(A) Right lateral and (B) ventrodorsal radiographs of a 10-year-old neutered male schnauzer with flail chest from unknown trauma. The dog had severe subcutaneous emphysema, segmental fractions of the left 5th and 6th ribs, and a transverse fracture of the proximal left 7th rib. Left-sided pneumothorax and an alveolar pattern in the left cranial lung lobes were also noted.
Physiology
During normal respiration, changes in pressure gradients cause air to move in and out of the lungs. During inspiration, the diaphragm and intercostal muscles contract, causing loss of concavity of the diaphragm and abduction of the ribs, respectively. Lung pressure then falls below atmospheric levels and creates a negative gradient that pulls air into the alveoli.
As air fills the lungs, the pressure reaches atmospheric levels and air flow stops. The lungs then exhibit elastic recoil, which creates positive pressure in the alveoli that causes air to move out of the lungs during expiration.2
In flail chest cases, the negative pressure gradient that normally pulls air into the lungs also exerts this force on the freely movable flail segment, causing inward displacement of the segment. This results in pain and decreased intrapleural space, which limits lung expansion. Similarly, the positive pressure generated during expiration pushes the segment outward. This abnormal movement produces the paradoxical motion—or _flailing—_that is typical of the condition.3
In dogs, experimentally induced flail chest not associated with pleural damage can result in respiratory abnormalities consequential to pain and decreased lung expansion. These abnormalities can include tachypnea, decreased minute volume, and decreased tidal volume. Such cases do not, however, cause hypoxemia or hypercapnia.4 This suggests that mortality in patients with flail chest is likely a result of concurrent injuries.
Diagnosis
Diagnosis is typically based on visualization of paradoxical movement of the fractured rib segment(s). Thoracic radiography can be used to definitively identify affected ribs and any additional injuries. Concurrent pneumothorax and pulmonary contusions are identified on radiographs in >50% of dogs with flail chest resulting from thoracic bite wounds.1
CT scans can provide more specific information about the extent of the injuries (Figure 2); however, CT requires deep sedation or general anesthesia, which limits its use in patients with marked respiratory distress.6
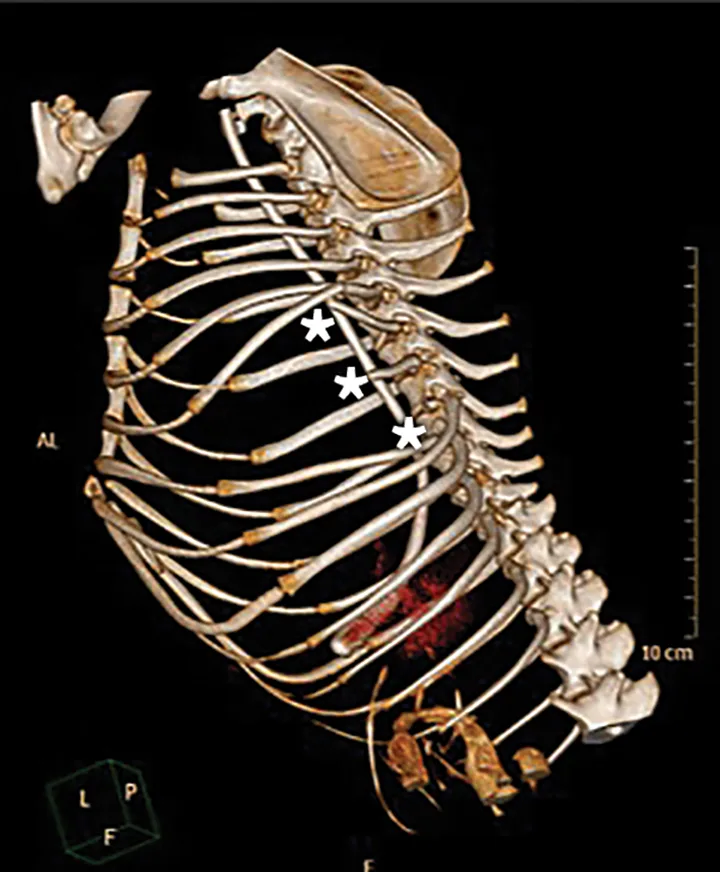
CT reconstruction of the thoracic skeleton of a 4-year-old female dachshund with apparent left-sided flail chest after an attack by another dog. The patient suffered a combination of proximal single and segmental fractures and luxations of ribs 6 through 11 on the left side (asterisks). Severe displacement of the ribs, along with extensive soft-tissue trauma, permitted paradoxical motion of the thoracic wall soft tissue.
Emergency Stabilization
Because flail chest is created by acute trauma, patients are often presented in shock. Patient stabilization is priority; standard triage procedures should be used to assess airway, breathing, and circulation. Supplementary oxygen should be provided and an IV catheter placed for fluid and analgesic administration.
Clinical Findings of Flail Chest
Clinical findings of flail chest can include5:
Tachypnea or dyspnea
Thoracic pain
Paradoxical inward displacement during inhalation and outward displacement during exhalation
Subcutaneous emphysema secondary to trauma
Hemoptysis
Intra-alveolar and interstitial hemorrhage
Hypoventilation
Hypoxemia
Pneumothorax
Pneumomediastinum
Pleural effusion
Patients may require fluid resuscitation with crystalloids with or without colloids. In dyspneic patients, oxygenation and tissue perfusion can be assessed via pulse oximetry, measurement of blood gases, and serial blood lactate concentrations. In intubated patients, end-tidal CO2 measurements can be used. Some patients may have concurrent pulmonary contusions and pneumothorax,3 so a thoracic-focused assessment with sonography for trauma can be performed to provide diagnostic information and facilitate thoracocentesis when indicated. Markedly dyspneic patients can be imaged in sternal recumbency.
When ultrasonography is not available, a diagnostic bilateral thoracocentesis may be pursued to diagnose and treat pneumothorax.7,8 In patients with tension pneumothorax (ie, buildup of air in the pleural space that results in positive intrapleural pressure) or in those that require 2 or more therapeutic thoracocenteses, thoracostomy tubes should be placed.8
After thoracocentesis, a chest wrap can be placed over the flail segment and around the thorax (see Step-by-Step: Bandaging for Flail Chest) if a chest tube or open wound is present. Potential benefits of thoracic stabilization include decreased motion of the flail segment, reduced pain, and decreased risk for lung and intercostal vessel laceration.5
Patients with flail chest require aggressive pain management. Many benefit from a pure -agonist (eg, fentanyl, hydromorphone), but analgesia should be selected on a case-by-case basis. Fast- acting, multimodal combinations (eg, fentanyllidocaine, morphinelidocaineketamine) delivered as a constant-rate infusion and titrated to effect are useful.8,9 Intercostal or epidural nerve blocks may also be beneficial.10
Open wounds should be clipped, cleaned, and covered with sterile dressings, and affected patients should be started on broad-spectrum antibiotics (eg, amoxicillinclavulanic acid, ampicillinsulbactam).11
Treatment
Treatment options include conservative therapy or surgical stabilization of the flail segment. Conservative management can be successful in many patients. Surgical stabilization should be considered if clinical signs do not resolve or if the patient is undergoing a thoracotomy for other conditions (eg, lung lobe laceration).
Conservative Treatment
Bandaging to cover any wounds and provide structural support to the chest
Surgical Therapy
Closed external stabilization of the flail segment with a splint by using towel clamps or circumcostal sutures passed percutaneously
Open stabilization of rib fractures with Kirschner wires, small intramedullary pins, screws, intersegmental wire placement, or absorbable polylactic acid plate and screws12
Removal of rib fragments (to prevent migration into viscera) and stabilization of the local soft tissue with suture, muscle flaps, and/or implants (eg, mesh)
Treatment Controversies
Controversy surrounds the most appropriate treatment of severe rib fractures and flail chest. In humans, surgical stabilization of flail chest reduces ventilatory support, intensive care unit stays, duration of hospitalization, incidence of pneumonia and septicemia, risk for chest deformity, and overall mortality as compared with internal pneumatic stabilization (ie, mechanical ventilation), percutaneous rib fixation, and other nonsurgical treatments.13 In patients with fractured ribs that do not require ventilation, the use of taping or strapping raises concerns about thoracic wall restriction, which could lead to pneumonia and further fracture displacement.14
Two small, randomized studies of rib belting in humans reported conflicting results. In one study, patients using rib belts and receiving analgesia experienced significantly greater pain relief and had no difference in pulmonary function testing as compared with patients only receiving analgesics.15 However, patients with displaced fractures using rib belts experienced a higher rate of hemothorax. In the other study, use of rib belts did not significantly decrease pain severity and may have increased the risk for atelectasis by restricting motion.16
Similar comparisons have not been conducted in dogs and cats. Bite wounds are a common cause of flail chest in these species,3 so bandaging is required for wound management in many patients. If bandages are used, they should not restrict ventilation.
In the author's hospital, padded bandages are placed on patients with open wounds or chest tubes and are used occasionally for flail segment stabilization, depending on clinician preference. In the latter case, bandages are used primarily to improve pain control and ventilation and are removed if SPO2 or blood gases worsen with application. If no wounds are present, bandages are removed in 2 to 3 days unless protection from self-trauma or housemates is needed.
Outcome
In one retrospective study, the overall mortality rate for dogs and cats was 17%3; the exact cause of death was unknown in many of the animals and may have been related to concurrent conditions (eg, disseminated intravascular coagulation, infection).
One study involving 24 dogs and cats undergoing treatment for flail chest showed mortality rates for conservative management and surgical treatment with internal or external stabilization of 6.3% and 33%, respectively.3
Step-by-Step: Bandaging for Flail Chest
What You Will Need
Wound-care materials (eg, clippers, gloves, chlorhexidine scrub and solution, sterile gauze, topical dressings)
Packing material (eg, gauze sponges, roll gauze, laparotomy pad)
Adhesive drape or skin tape to hold packing in place
Cast padding
Roll gauze (optional)
Nonadhesive wrap for a tertiary layer
Step 1
After the patient is stabilized, clip and clean any external wounds. Cover the wounds with an appropriate topical antimicrobial and sterile dressing.

Step 2
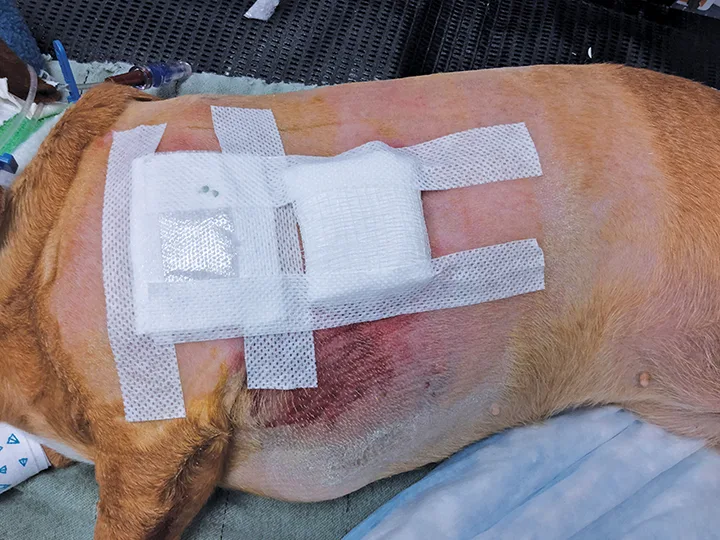
Place wound dressings over any open wounds. Secure them in place with skin tape.

Step 3
Place a small amount of padding over the flail segment to keep the area level with the surrounding thoracic wall and reduce paradoxical motion. Secure the padding with skin tape.
Step 4
If wounds are present, place an adhesive drape over the area. This will keep the padding in place and allow wound dressings to be evaluated for strike-through. If strike-through occurs, remove the drape over the wound dressing; change the dressing and replace that portion of the adhesive drape.

Step 5
As an alternative, apply cast padding around the chest and between the forelimbs; cover with a self-adhesive tertiary wrap. The wrap should be snug but should not limit respiration. To prevent excessive compression, unroll and reroll bandage material before use.

Author Insight
If the wounds require frequent bandage changes, place the wrap in 2 stages so the portion overlying the flail segment or chest tube, if present, does not need to be removed with the remaining bandage.