Fiber-Responsive Diarrhea

You have asked… How do I nutritionally manage a patient with fiber-responsive diarrhea?
The expert says… Some cats and dogs presented for diarrhea can be managed with diets containing particularlevels and types of fiber. Determining a patient's exact fiber needs may involve trial anderror. Client guidance and compliance also plays a role in successful management.
Related Article: Treatment of Chronic Gastrointestinal Disease
Initial Approach
A detailed patient history may help diet selection or suggest an underlying cause. Review of all previous diets, treats, chews, table scraps, and routes of medication administration can help ruleout coincidental dietary indiscretion or food items at risk for bacterial contamination (eg, chews, raw food diets).1,2 Dietary history forms can be found online.3
Medical history may suggest which aspects of the GI tract are affected (eg, increased frequency, urgency, frank blood, or mucus in stool suggesting a large intestine issue), which may assist in identifying the type of fiber supplementation needed.
A detailed patient history may help diet selection or suggest an underlying cause.
Discussing the home environment may also guide management. For example, a pet having diarrhea every time a family member leaves for an extended period may indicate colitis brought on by stress. For chronic or severe cases, a full diagnostic evaluation, including imaging or a dietary elimination trial, may be indicated. Many GI diseases have similar clinical presentations (see Table: Additional Differentials to Consider).
Fiber Explained
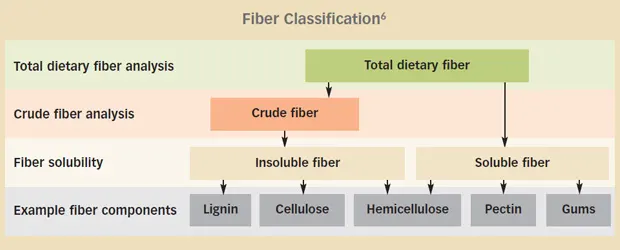
The term high fiber can be confusing, as fiber is added and analyzed in various ways. Fiber is commonly categorized according to solubility or fermentability. Although many soluble fibers are also highly fermentable, solubility refers to the ability of a fiber to disperse in water, whereas fermentability characterizes the rate at which fibers can produce short-chain fatty acids (SCFAs).

Insoluble fibers (eg, cellulose) provide increased fecal bulk that can stimulate GI motility and increase intestinal transit time. Because added insoluble fiber can mildly alter nutrient digestibility,4,5 caution should be taken if supplementing large amounts; diets may not be formulated to account for a decrease in nutrient digestibility. Insoluble fiber is common in diets formulated for diabetes or weight management in dogs and weight management and hairball control in cats.
Soluble fibers (eg, pectins, gums) have a greater capacity to absorb water and tend to be highly fermentable. Highly fermentable fibers are rapidly converted by bacteria to SCFAs, the preferred energy source for colonocytes. These fibers can promote healthy colonic mucosa and immune function. Supplementation should be done slowly and incrementally; because of its ability to absorb water, patients may experience worsening of diarrhea if too much soluble fiber is added rapidly.
Oligosaccharides are fermentable carbohydrates (also called prebiotics) often used because of their ability to foster beneficial bacteria in the GI tract.
Patients must be treated on an individual basis when considering the amounts of each fiber type (see Fiber Classification6) in a diet. Psyllium, a soluble fiber, has shown benefits in the treatment of chronic idiopathic large bowel diarrhea in dogs7 and constipation in cats.8 A history of previous diets may guide whether a higher percentage of insoluble or soluble fiber can benefit the patient. If this is unclear, an initial trial with a moderate mixed-fiber diet containing both insoluble fiber sources (eg, cellulose) and soluble sources (eg, gums) with total dietary fiber less than 10% on a dry-matter basis can be initiated.9
Nutrient Profile
Barring a proven food allergy, the overall nutrient profile should determine the diet instead of individual ingredients. Low-fat, highly digestible diets are commonly recommended for intestinal disease9; however, a study in cats showed that dietary fat content did not affect clinical outcome,10 underscoring the need for individualized dietary management.
In addition, because diets low in fat and high in fiber may have a lower caloric density, diets should be selected based on specific energy needs of each patient. An underweight dog, for example, may have difficulty consuming enough low-calorie food to maintain its weight.
Evaluation should be based on total dietary fiber (TDF), which includes soluble and insoluble fiber, on an energy (grams/megacalorie) or dry-matter basis to compare diets of differing caloric or moisture content. The maximum or minimum guaranteed analysis of crude fiber on pet food labels only accounts for some insoluble fibers on an as-fed (by weight) basis.
A typical nutrient analysis of TDF can be found in company product guides or by contacting the manufacturer. Although an ingredient list may show soluble or insoluble fiber ingredients, the total amount is unknown without the TDF and crude fiber in the nutrient profile.
Fiber can be supplemented, but there is limited evidence for standardized dosing. One study using a common human psyllium supplement found beneficial effects in dogs receiving a median dose of 2 tablespoons q24h (range, 0.25–6 tablespoons q24h).7 In the author’s experience, fiber should always be supplemented in gradual increases of approximately 1 teaspoon per day to desired stool composition, which may require a few days of supplementation.
Canned pumpkin is a common fiber additive used by clients, but the amount needed for clinical benefit may unbalance the total diet (>10% of total calories; see Tips for Guiding Clients). Probiotics are another common supplement, but quality control varies.11
SCFAs = short-chain fatty acids, TDF = total dietary fiber
DEBORAH LINDER, DVM, DACVN, is head of Tufts Obesity Clinic for Animals and volunteers with Tufts Paws for People Animal Visitation Group. Her interests include obesity management and client education. Dr. Linder’s research investigates safe and effective weight loss strategies for pets and the effects of obesity on animal well-being. Dr. Linder earned her DVM from Tufts Cummings.