Feline Tracheal Tumors: Uncommon or Overlooked?
You have asked…
What do I need to consider when presented with a feline patient in respiratory distress to prevent a delayed or missed diagnosis of tracheal neoplasia?
The experts say…
Facing a dyspneic feline patient can be intimidating for veterinarians and frightening for owners. There are many causes of feline respiratory distress, but one that receives little attention is tracheal neoplasia. Feline tracheal tumors are infrequently reported.1 As such, clinical suspicion is typically low, and there is a paucity of recommended diagnostic and treatment plans for feline tracheal tumors.
Related Article: Respiratory Distress in a Cat
The scarcity of reported or confirmed feline tracheal tumors is mirrored in human literature, where 2% of respiratory tract tumors are reported to originate from the trachea.2 No predisposing causes are known for tracheal neoplasia.3 One hypothetical factor responsible for limiting neoplastic invasion may be the unique anatomic morphology of the trachea, which includes a patent rigid lumen with dynamic airflow and kinociliary respiratory epithelium. Unrecognized immunologic defenses may also provide antineoplastic protection. In a case series exploring feline upper airway tumors, laryngeal tumors were 3 times more common than tracheal tumors.4 This, too, is reflected in the human literature, with a large retrospective study reporting that development of laryngeal tumors is 40 times more likely than tracheal tumors.5 It is not understood why this prevalence disparity exists in spite of similar anatomic topography.
Epidemiology
Cats with tracheal tumors are typically middle-aged patients (median age, 9.5 years; range, 2–13 years), and there is no known sex predilection.6 Interestingly, dogs with tracheal tumors show a bimodal age distribution, with presenting signs noted before 2 and after 6 years of age.6 This pattern results from the variance in tumor types of different age groups. Younger canine patients may be diagnosed with benign osteochondroma; older patients are at risk for adenocarcinoma and chondrosarcoma, among others.4 Domestic short-haired cats are overrepresented in reports of tracheal tumors, but this may be the result of a disproportionate population bias.7 An overrepresentation of Siamese cats with tracheal lymphoma has been reported; however, no other breed predispositions were noted.6,7
Clinical Signs
There are no pathognomonic signs that signal the presence of feline tracheal tumors. The most common presenting complaints include dyspnea, stridor, wheezing, dysphonia, and coughing.6,7 These nonspecific signs present a challenge to veterinarians as they mimic other diseases. The insidious nature of tracheal tumors may also present a diagnostic and therapeutic challenge. Cats with tracheal tumors often receive supportive treatment for general respiratory illness, which results in delayed intervention and progression of clinical disease. Moreover, 40% to 50% of the tracheal lumen can be occluded before clinical manifestations of the disease are recognized.8
Related Article: Diagnosing Feline Respiratory Disease
Diagnostics
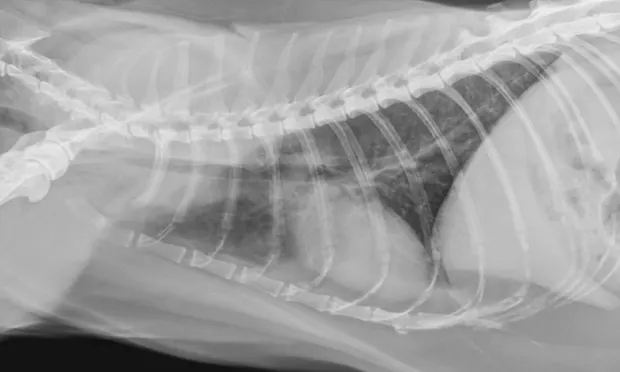
Figure 1. Thoracic radiographs performed on a cat with mixed respiratory signs. Moderate bronchial and mild unstructured interstitial pulmonary patterns consistent with nondescript chronic airway disease and age-related changes can be observed.

A thorough physical examination, including tracheal palpation, auscultation, and a laryngeal examination, are paramount to early detection of upper respiratory tumors in cats with nonspecific respiratory illness.
Radiographs remain the most widely available screening modality for identification of tracheal neoplasia.7,9,10 Air provides an excellent natural contrast medium for diagnosis of tracheal masses. Cats with tracheal tumors may have concurrent lung pathology. Thus, the presence of lower respiratory disease should not preclude evaluation for tracheal tumors if clinical suspicion exists. Failure to pursue additional imaging, including cervical and thoracic radiographs, may lead to a misdiagnosis or delay in therapy (Figures 1 and 2).
Figure 2. Cervical radiographs performed on the same cat as in Figure 1. A large cervical tracheal mass (arrow) occluding approximately 90% of the trachea at C3–C5 can be observed.

Studies have shown no significant difference in tumor predilection for the cervical trachea vs the intrathoracic trachea. Esophagrams provide an additional inexpensive diagnostic test. This modality aids in the identification of tracheal tumors through exclusion of artifacts, including esophageal superimposition and extraluminal compression from surrounding structures.11 Tracheoscopy and computed tomography provide information for surgical planning and assessment of peritracheal invasion.11,12
Treatment
Treatment options should be individualized for each patient and considerate of the owners’ expectations. Given the generally low metastatic rate, aggressive surgical intervention is recommended when the mass is deemed resectable (with the exception of primary lymphoid tumors).2,3,13 Resection and anastomosis are possible for tumors located in both the cervical and thoracic trachea. Historically, surgical planning has allowed for removal of 50% of the trachea without secondary stenosis.8 However, a more recent study suggests that although tracheal diameter remains unaffected, negative changes to the luminal diameter of lobar bronchi occur with ≥30% tracheal resection and anastomosis procedures.14
Although supportive therapies rarely result in resolution of clinical signs, the tumor location, concurrent comorbidities, anesthetic risks, financial constraints, and owner expectations may limit aggressive treatment.
Endoscopic debulking using a wire snare is also described and may afford prolonged survival without the need for concurrent medical management. Moreover, it may provide immediate clinical relief.9 Debulking is not without risk as tracheal tumors may be highly vascular and invasive. Therefore, associated complications can include intraluminal hemorrhage and cervical or mediastinal emphysema if a full-thickness hole in the tracheal wall is made. Clients should be informed that debulking procedures are palliative, and recrudescence of disease should be anticipated.
Chemotherapy and radiation can be considered but require a definitive diagnosis. These treatment options are typically reserved for tumors of lymphoid origin, where they are considered to be the treatment of choice. Similar to endoscopic debulking, chemotherapy and radiation are considered palliative.
Tracheal stenting is a palliative treatment that can be offered to patients when surgery is not an option.15 Progression of disease should be anticipated in these cases. Therefore, stents should not to be considered a first-line therapy. Stent placement has been described in a small population of cats with benign and neoplastic causes of tracheal narrowing.16 No complications followed these procedures, but well-documented risks in humans include stent dislodgement and stricture formation.15
Related Article: Heartworm-Associated Respiratory Disease in Cats
Supportive Care
Advanced disease often dictates the choice of supportive care for cats with tracheal tumors. Although supportive therapies rarely result in resolution of clinical signs, the tumor location, concurrent comorbidities, anesthetic risks, financial constraints, and owner expectations may limit aggressive treatment. Supportive care options include antiinflammatory drugs, antibiotics for secondary bacterial infections, and bronchodilators. Routine veterinary evaluations and client education to recognize worsening clinical signs cannot be overemphasized. Progressive tumor growth puts cats at high risk for acute respiratory distress. A thorough client discussion is a necessity to ensure patients are closely monitored for progressive disease.
Prognosis
The limited number of reported cases makes prognostication difficult. Survival may be influenced by treatment selection; however, the overall prognosis for cats with tracheal tumors is guarded. Jakubiak et al demonstrated an overall median survival time of cats with malignant laryngeal and tracheal tumors of 15.5 days (1–1109 days).7 Reported survival times for surgical resection and endoscopic debulking of tracheal tumors ranged from 3–35 months and 1–35 months respectively.9,10,17 In a case series, chemotherapy and radiation treatment in 2 cats with lymphoma provided remission and long-term resolution of clinical signs for 17 and 19 months, respectively.18 Survival times for supportive care are difficult to assess because of challenges associated with consistent patient follow-up and limited published data.
Conclusion
Cats with tracheal tumors are presented with nonspecific clinical signs and are likely under-recognized. Erroneous clinical assessment and recognition may lead to delayed treatment and decreased survival rates.5 Prompt therapeutic intervention requires appropriate clinical suspicion and diagnostics. Widely available imaging modalities, including cervical, thoracic radiographs, and contrast esophagrams, aid in the diagnosis of tracheal neoplasia. Multiple treatment options exist, including surgical resection, interventional debulking, chemotherapy and radiation, and supportive care. Appropriate patient selection, diagnosis, treatment choice, and owner education may result in a better prognosis than previously reported.
JAMES HOWARD, DVM, is small animal medicine and surgery rotating intern at University of Tennessee. His diverse interests include respiratory diseases and multi-modal treatment protocols for critical patients. Dr. Howard graduated from Ohio State University.
M. KATHERINE TOLBERT, DVM, PhD, DACVIM, is assistant professor at University of Tennessee, where her laboratory focuses on using cell-based models to characterize pathogenic mechanisms of enteric infections and exploring novel therapies to prevent and/or ameliorate infectious enterocolitis in cats. Her varied clinical research includes studies of respiratory disease, acid-related disorders, and GI infections. A graduate of University of Georgia, where she completed a small animal internship, Dr. Tolbert completed a small animal internal medicine residency and a comparative biomedical sciences doctorate at North Carolina State University.