Feline Oropharyngeal Inflammation
You have asked…
Generally any significant inflammation in the cat’s mouth is called stomatitis. Is this correct?
The expert says…
Cats with oral inflammation can be among the most frustrating patients veterinarians manage. Even the terminology for this condition is problematic and confusing. For years, almost any inflammation of the feline oral cavity was termed stomatitis. This term is still used, but only to describe widespread inflammation of the oral cavity as opposed to gingivitis or periodontitis, which involves localized support loss andmucositis.
In August 2009, the American Veterinary Dental College approved the term oropharyngeal inflammation to refer to any type of oral inflammation. Inflammation is then further classified according to location (see Classifying Oral Inflammation).
Pathogenesis
The cause of oropharyngeal inflammation has not been definitively determined. A multifactorial cause is suspected, including genetic predisposition, environmental stress, diet, and viral (calicivirus, herpesvirus1-3) and bacterial (Bartonella species) infection. In addition, dental plaque intolerance is thought to be involved. Cats with oropharyngeal inflammation have an inadequate or an exaggerated immune response, which leads to markedly inflamed gingiva and oral mucosa.
History & Clinical Signs
The median age of cats with oropharyngeal inflammation is 7 years. A patient’s history often includes dysphagia or anorexia that has caused weight loss, ptyalism, bruxism (teeth grinding), and face pawing. The cat may avoid opening its mouth when eating. The cat’s coat is often unkempt because of poor self-grooming due to oral pain. Halitosis and bleeding within the oral cavity are common. Glossitis, cheilitis, and mandibular lymphadenopathy may also be evident. Widespread inflammation of the palate and pharynx is usually not present.
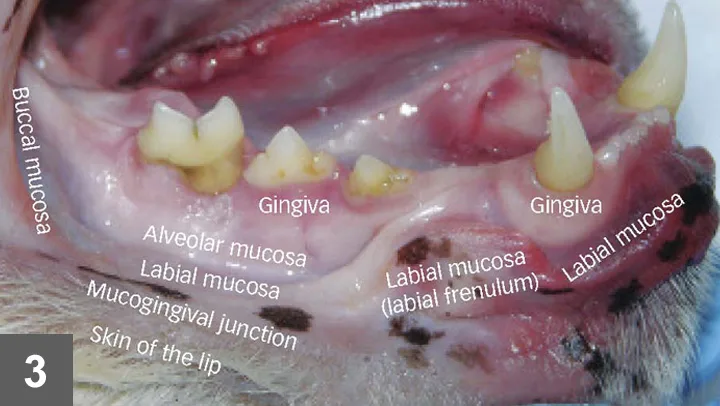
In some cats, inflammation is apparent only around the caudal cheek teeth, extending from the gingiva beyond the mucogingival junction into the alveolar mucosa. Other cats show marked gingivitis and periodontitis 360 degrees around the incisors, premolars, or molars.
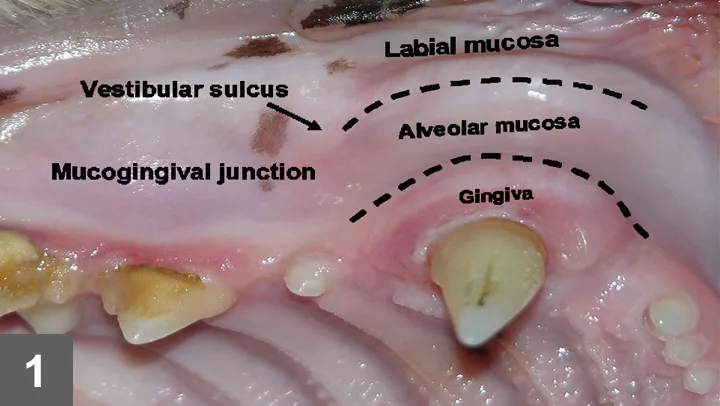
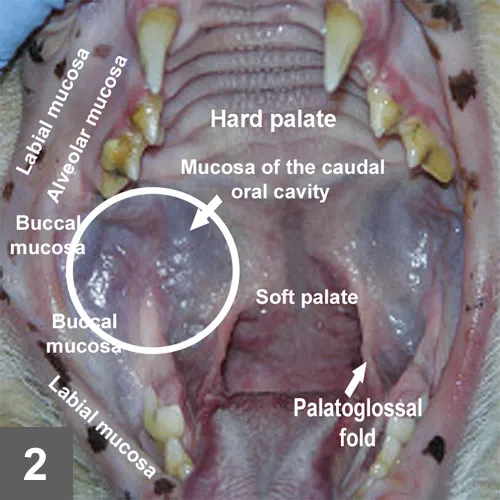
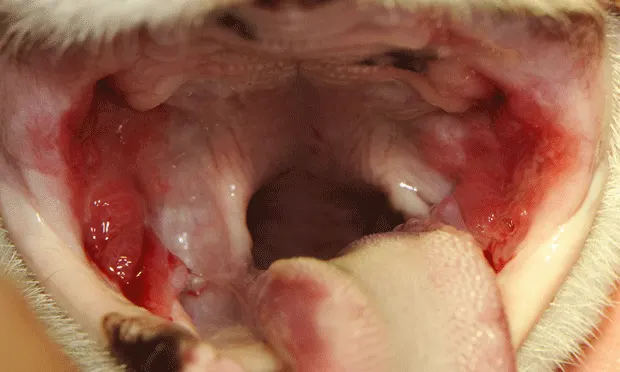
Before there was stomatis: In the past, stomatitis was called lymphoytic-plasmacytic gingivostomatitis as well as plasma cell gingivitis, faucitis, and pharyngitis; the latter 2 terms are incorrect because the fauces and pharynx are normally not involved in stomatitis. For a refresher on dental anatomy, see Figures 1 through 3. (view larger image)
Caudal stomatitis clinically appears as cobblestone-like, ulcerative, proliferative, hyperemic lesions that involve the palatoglossal folds and regions lateral to the folds. It is present in 85% of cats affected by chronic oropharyngeal inflammation. One study found that 15% of the cats had only caudal stomatitis without apparent lesions further rostrally.4
Diagnosis
Histopathologic examination of the mucosa and submucosa reveals dense infiltrations of plasma cells with lesser numbers of lymphocytes, neutrophils, and macrophages, consistent with almost any inflammation in a cat’s mouth. Unfortunately, the only advantage of histopathologic testing is to rule out neoplasia.
Treatment
Tooth Extraction. Supragingival and subgingival plaque appears to be one of the multifactorial initiating sources of oropharyngeal inflammation. In most cats with widespread oropharyngeal inflammation, tooth extraction, which decreases the plaque burden, is the only treatment that is associated with long-term positive results and does not necessitate further medication. The decision of whether to extract all teeth or only premolars and molars is based on examination findings. If marked inflammation, periodontal pockets, or tooth resorption is noted around the canines or incisors, these teeth are also extracted.
Presurgical radiographs are important to evaluate root anatomy and pathologic abnormalities. Teeth with resorptive lesions are often undergoing root replacement resorption, making luxation and elevation difficult. These teeth should be treated by amputating the crown and suturing the gingiva. Pulverizing or atomizing the root within the alveolus with a water-cooled, high-speed handpiece and dental burr may remove excess supporting bone, remove too little tooth, or cause trauma to adjacent anatomy; this technique should be avoided. If any teeth remain after the procedure, a plaque preventive agent (eg, OraVet, merial.com) should be applied.
Response to Treatment. To evaluate the response to extraction in cases of chronic caudal stomatitis, a retrospective study assessed dental extractions in 30 cats with calicivirus.4 In that study, 60% of the cases resolved without need for further treatment, 20% significantly improved and required less medication to control stomatitis than before extractions, 13% improved but required similar amounts of continuing antiinflammatory treatment, and 7% did not improve after receiving medical or surgical care.
Nutritional Support & Pain Management. For anorectic patients that present in poor condition, nutritional support through a pharyngostomy or gastrostomy tube is indicated before or after surgery, or both, until the patient’s appetite returns to normal.
In surgical patients, pain is managed with preanesthetic administration of an opioid (buprenorphine, 0.01–0.02 mg/kg IM, SQ, transmucosal),5 intraoperative local anesthetics (bupivacaine, 1–2 mg/kg), and postoperative opioids given orally for 5 to 7 days.
Monitoring
Postoperative examination is performed 2 weeks after surgery. It is important to show the client how to control plaque on any remaining teeth by using 0.12% chlorhexidine gluconate irrigation daily and OraVet application weekly.
When oropharyngeal inflammation persists for months despite extractions, extraction of all remaining teeth and root fragments is indicated. If lesions persist and the patient has been affected for months to years, the condition is termed refractory oropharyngeal inflammation. Removing multiple teeth and root fragments, together with periodic laser thermoablation and medication (prednisone, 0.5 mg/kg Q 2–3 days), may be helpful in these cases.

Alveolar Mucositis
Inflammation of the alveolar mucosa (the mucosa overlying the alveolar process and extending from the mucogingival junction to the vestibular sulcus and floor of the mouth).