Exophthalmos in a Dog
An 8-year-old, 4.8-kg, spayed female dachshund presented with a 4-day history of progressive, bilateral exophthalmos.
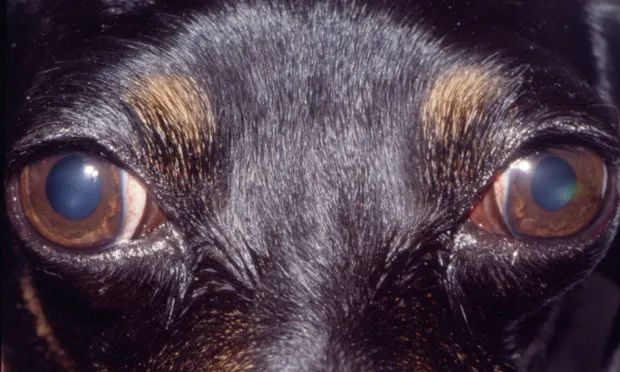
Physical Examination. No pain or restriction was detected when opening the mouth. No pain, atrophy, or swelling of the temporalis or masseter muscles was noted. Complete ophthalmic examination revealed bilateral restrictive exophthalmos and nictitans elevation with slight exotropia (OD > OS), superficial corneal erosion OS, mild anterior uveitis OS, and distichiasis OU (Figure 1, above).
Figure 1. Bilateral extraocular photograph of the patient showing bilateral exophthalmos, slight exotropia (OD > OS), and bilater al elevation of the thir d eyelid. A focal, axial, superficial corneal erosion was also present in the left eye
Initial Diagnostics**.** Results of a CBC, chemistry profile, serum creatine phosphokinase (CK), and urinalysis were normal. Total thyroxine (T4) and triiodothyronine (T3), free T3 and T4, T3 and T4 autoantibodies, and thyroid-stimulating hormone levels were normal. Serum IgG titers for Blastomyces dermatitidis, Histoplasma capsulatum, Cryptococcus neoformans, Neospora caninum, and IgG and IgM titers for Toxoplasma gondii were negative.
Lupus erythematous and antinuclear antibody testing were negative. The patient's fresh frozen serum was incubated with normal canine extraocular muscle and staphylococcal protein A conjugated with horseradish peroxidase (SPA-HRPO), then stained for peroxidase localization.1 No labeling of myofiber components was observed. Serology for type 2M myofibers was negative.<sup2, 3sup> Thoracic radiographs demonstrated no evidence of neoplasia or fungal disease.
ASK YOURSELF ...What additional diagnostic testing should be pursued?A. Schirmer's tear test and rose bengal stainB. Ultrasonography, CT, and muscle biopsyC. Fluorescein stain and intraocular pressure measurementD. Conjunctival biopsyE. Gonioscopy with scleral depression
Correct Answer: BUltrasonography, CT, and muscle biopsy
Diagnostic imaging techniques are often useful in the diagnosis of exophthalmos (protrusion of the globe out of the orbit). In this patient, ocular ultrasound revealed markedly swollen extraocular muscles OU (Figure 2) with homogeneous low-reflective enlargement, suggestive of myositis.4-7

Figure 2. Ocular ultrasonography of the right eye. Note the markedly swollen extraocular muscles (arrows) with homogeneous low-reflective enlargement, diagnostic of myositis. The appearance of the left eye was similar.
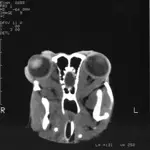
Head CT and extraocular muscle biospy were performed under general anesthesia. Enlargement of the extraocular muscles was apparent OU (Figure 3). No bone lysis, soft tissue mineralization, orbital fractures, foreign bodies, or other abnormalities were detected. Open extraocular muscle biopsy was performed. Dorsal rectus muscle with tendenous insertion (7 mm × 1 mm) was harvested from the lateral one third of the muscle belly.5 Fixed and frozen biopsy sections were submitted for complete muscle profiles. These biopsies showed myofibers and dense
connective tissue mixed with cellular infiltrates (lymphocytes, macrophages, and scattered eosinophils) in an endomysial distribution (Figure 4).
Figure 3. A 43° oblique dorsal plane CT image. This technique was used to optimize extraocular muscle imaging. Abnormalities were limited to bilateral extraocular muscle enlargement.
Figure 4. Photomicrograph demonstrating the histologic characteristics of the dorsal rectus muscle biopsy. Myofibers infiltrated with lymphocytes, macrophages, and scattered eosinophils in an endomysial distribution are seen. (Hematoxylin andeosin stain; magnification 20¥
Diagnosis. This patient's clinical signs, signalment, medical history (previously healthy and current on vaccinations and heartworm prevention), and regional habitat (Midwest), coupled with the results of ophthalmic examination, were highly suggestive of bilateral extraocular polymyositis (BEP). The most likely cause of the focal, axial corneal erosion OS was exposure keratitis secondary to the lagophthalmos.8
Orbital myositis is a well recognized, idiopathic inflammatory condition involving one or more extraocular muscles.<sup4, 5, 9-14sup> Canine bilateral extraocular polymyositis is a unique type of orbital myositis characterized by a mononuclear inflammatory cell infiltrate of all extraocular muscles except for the retractor bulbi.8,15,16 When supportive clinical findings are present, diagnosis is based on several criteria: Masticatory muscle myositis should be ruled out based on normal CK levels and lack of autoantibodies against type 2M myofibers in extraocular tissue sections and patient sera.<sup2, 8, 17, 18sup> Normal thyroid function should be established; other systemic infectious, autoimmune, or neoplastic disease should be excluded; imaging studies should demonstrate abnormalities limited to the extraocular muscles; and characteristic extra-ocular muscle histology should be documented.<sup8, 16, 19-27sup> Exact etiology of BEP is currently unknown; however, an autoimmune pathogenesis has been proposed based on pattern of muscle involvement, pathologic characteristics, and response to therapy.15,16
Differential Diagnosis**.** Differential considerations for canine exophthalmos are numerous. This condition may result from primary orbital conditions or secondary to disease extension from surrounding tissues, including the oral cavity, muscles of mastication, brain, globes, nasal sinuses, or mandibular ramus.<sup17, 28-34sup>
Treatment. Objectives were to resolve the extraocular myositis and prevent additional muscle fibrosis by treating with immunosuppressive agents, minimize exposure keratitis OU, prevent secondary corneal infection OS, and treat the reflex uveitis OS.
Initial treatment consisted of prednisone (1 mg/kg PO Q 12 H), azathioprine (2 mg/kg PO Q 24 H), triple antibiotic ointment (OU Q 6 H), atropine (OS Q 24 H for 3 days), and an Elizabethan collar to prevent self-trauma. Prednisone and azathioprine were initiated concurrently due to histologic evidence of sclerosing inflammation. Immunoregulatory agents such as cyclophosphamide, azathioprine, methotrexate, and/or cyclosporine, in combination with corticosteroid therapy, may reduce the amount of fibrosis and cicatricial sequelae to this type of extraocular inflammation.5

Outcome. Two weeks after initial presentation, complete ophthalmic examination revealed marked improvement in exophthalmos, ocular motility, and retropulsion OU. Clinical evidence of BEP was resolved by 3 weeks.
Serial CBC and serum chemistry panels were monitored for side effects from systemic therapy. Prednisone taper began at 3 weeks; the drug was discontinued at 8 weeks. Azathioprine was slowly tapered and was discontinued at 10 weeks. Caution should be exercised to avoid tapering immunosuppressive therapy too quickly, which imposes risk of a recurrence in clinical signs.
At 6 months, the dog had not received any medical therapy for 4 months, demonstrated no recurrence in BEP, had no restrictive fibrosis, and had good ocular motility OU (Figure 5). The patient is currently disease free but continues to be regularly monitored.
Figure 5. Bilateral extr aocular photograph obtained at 6-month recheck. No evidence of exophthalmos or corneal ulceration was seen OU. The dog had excellent ocular motility.
Take-Home Messages
Extraocular muscle myositis should be considered as a differential diagnosis in dogs presenting with sudden-onset bilateral exophthalmos.
Imaging modalities such as ultrasound, CT, and/or MRI are often very helpful in reaching a diagnosis, since swelling of the extraocular muscles is evident.
Patients generally respond favorably to immunosuppressive therapy, although recurrence is possible. Careful monitoring is warranted.
DIAGNOSING EXOPHTHALMOS IN A DOG • Elizabeth A. Giuliano
References
1. Fiber type-specific autoantibodies in a dog with eosinophilic myositis. Shelton GD, Cardinet GH, Bandman E, et al. Muscle Nerve 8:783-790, 1985.2. Canine masticatory muscle disorders: A study of 29 cases. Shelton GD, Cardinet GH, Bandman E. Muscle Nerve 10:753-766, 1987.3. Masticatory myopathy in the dog: A retrospective study of 18 cases. Gilmour MA, Morgan RV, Moore FM. JAAHA 28:300-306, 1992.
Idiopathic orbital myositis. Scott IU, Siatkowski RM. Curr Opin Rheumatol 9:504-512, 1997.5. Nonthyroid causes of extraocular muscle disease. Lacey B, Chang W, Rootman J. Surv Ophthalmol 44:187-213, 1999.
Orbital myositis involving the oblique muscles. An echographic study. Wan WL, Cano MR, Green RL. Ophthalmology 95:1522-1528, 1988.7. Orbital tissue differentiation with standardized echography. Byrne SR, Glaser JS. Ophthalmology 90:1071-1090, 1983.8. Exophthalmos. Ramsey DT. In Bonagura JD (ed): Kirk's Current Veterinary Therapy XIII-Philadelphia: WB Saunders, 2000, pp 1086-1089.9. Orbital myositis: A study of six cases. Hankey GJ, Silbert PL, Edis RH, et al. Austral N Z J Med 17:585-591, 1987.10. Orbital myositis-A case report. Barnes C. Austral N Z J Ophthalmol 18:251-255, 1990.
Acute recurrent orbital myositis. Ludwig I, Tomsak RL. J Clin Neuroophthalmol 3:41-47, 1983.12. Acute and subacute orbital myositis. Weinstein GS, Dresner SC, Slamovits TL, et al. Am J Ophthalmol 96:209-217, 1983.13. Extraocular muscle myositis and restrictive strabismus in 10 dogs. Allgoewer I, Blair M, Basher T, et al. Vet Ophthalmol 3:21-26, 2000.14. Bilateral proptosis caused by orbital myositis. A case report. Aydin K, Narin N, Erkilic K, et al. Turk J Pediatr 40:135-138, 1998.15. Canine bilateral extraocular polymyositis. Carpenter JL, Schmidt GM, Moore FM, et al. Vet Pathol 26:510-512, 1989.16. Clinical and immunohistochemical characteristics of bilateral extraocular polymyositis of dogs. Ramsey DT, Hamor RE, Gerding PA, et al. Proc Am Coll Vet Ophthalmol, 1995, pp 130-132.17. Diagnosing and treating masticatory myositis. Brogdon JD, Brightman AH, McLaughlin SA. Vet Med 86:1164-1170, 1991.18. Pathophysiologic basis of canine muscle disorders. Shelton GD, Cardinet GH. J Am Vet Intern Med 1:36-44, 1987.19. Thyroid ocular myopathy. Hodes BL, Shoch DE. Trans Am Ophthalmol Soc 77:80-103, 1979.20. Anaerobic orbital cellulitis and septicemia in a dog. Collins KB, Moore CP, Dubielzig RR, et al. Can Vet J 32:683-685, 1991.
Disseminated cryptococcosis with ocular involvement in a dog. Carlton WW, Feeney DA, Zimmerman JL. JAAHA 12:53-59, 1976.22. Orbital inflammation, myositis, and systemic lupus erythematosus. Grimson BS, Simons KB. Arch Ophthalmol 101:736-738, 1983.23. Metastatic small cell carcinoma masquerading as orbital myositis. Divine RD, Anderson RL. Ophthalmic Surg 13:483-487, 1982.24. Ocular changes in malignant lymphoma of dogs. Cello RM, Hutcherson B. Cornell Vet 52:492-523, 1962.25. Orbital myositis as a paraneoplastic syndrome. Harris GJ, Murphy ML, Schmidt EW, et al. Arch Ophthalmol 112:380-386, 1994.
Ultrasonography of the eye and orbit. Eisenberg HM. Vet Clin North Am Small Anim Pract 15:1263-1273, 1985.27. Computed tomography of extraocular muscle abnormalities. Haik BG, Saint-Louis LA, Smith ME. Intl Ophthalmol Clin 26:123-150, 1986.
Ophthalmic manifestations and complications of dental disease in dogs and cats. Ramsey DT, Marretta SM, Hamor RE, et al. JAAHA 32:215-224, 1996.29. Granular cell myoblastoma (schwannoma) in the orbit and cerebrum of two dogs. Holscher MA, Netsky MG, Lee TT, et al. Canine Pract 10:35-38, 1983.30. Ocular granulomatous meningoencephalitis in a dog. Ward DA, Kaswan RL, Martin CL. Proc Am Coll Vet Ophthalmol, 1987, p 307.31. Clinical presentation, morphology and behavior of primary choroidal melanomas in eight dogs. Collinson PN, Peiffer RL. Prog Comp Vet Ophthalmol 3:158-164, 1993.32. Magnetic resonance evaluation of intra and extracranial extension of nasal adenocarcinoma in a dog and cat. Voges AK, Ackerman N. Vet Radiol and Ultrasound 36:196-200, 1995.33. Computer tomographic imaging of nasal disease in 100 dogs. Burk RL. Vet Radiol Ultrasound 33:177-180, 1992.34. Unilateral exophthalmos and strabismus due to cranio-mandibular osteopathy. Dennis R, Barnett KC, Sansom J, et al. J Small Anim Pract 34:457-461, 1993.