Environmental Decontamination for Ringworm
Alison Diesel, DVM, DACVD, Texas A&M University
In the Literature
Moriello KA. Decontamination of 70 foster family homes exposed to Microsporum canis infected cats: a retrospective study. Vet Dermatol. 2019;30(2):178-e55.
The Research …
As part of successful treatment of dermatophytosis, environmental decontamination is recommended to eliminate infective material in the home environment. Although environmental contamination is considered an unlikely source of dermatophyte transmission, many pet owners may be fearful of persistent organisms in the environment and/or frustrated at the perception of difficult successful home decontamination.
This retrospective study evaluated the success of decontamination of homes in which Microsporum canis-infected cats lived as part of a foster program. Seventy homes were evaluated over a 10-year period as part of establishing a dermatophyte treatment program for shelters. Foster families were instructed to confine cats to a single room. Once the cat left the home, the environment was cleaned and sampled for residual contamination. The cleaning process involved removal of all visible debris, followed by wiping of surfaces with an over-the-counter household detergent. Once excess water was removed, all surfaces were disinfected with either 1:100 household bleach or 1:16 accelerated hydrogen peroxide.
Culture results were negative after a single cleaning in 38 of the 70 homes. In the other homes, complete decontamination was achieved after an additional 1 to 3 cleanings. Cultures were taken from furnace filters and room vents in 9 homes and were all negative. There were no reports of dermatophyte transmission to animals or humans during the study period.
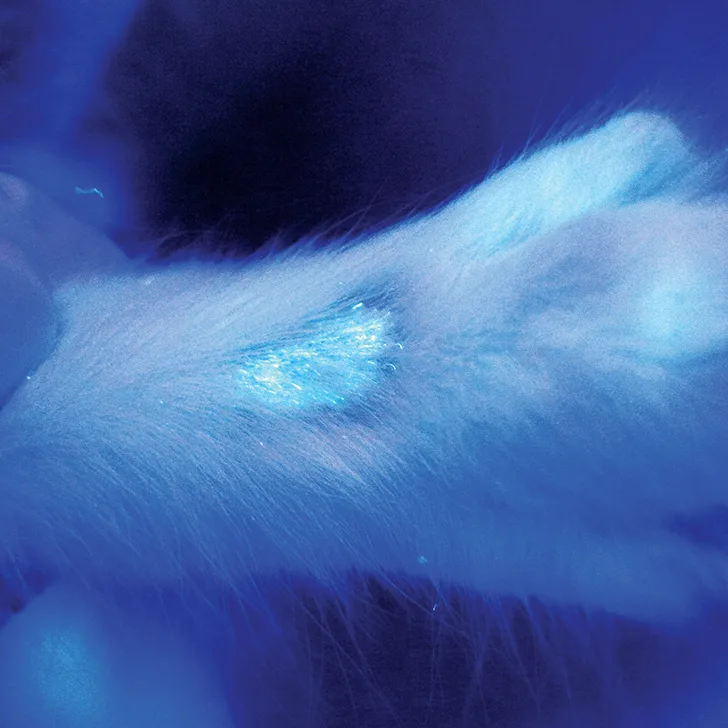
Positive Wood’s lamp fluorescence result in a kitten with Microsporum canis dermatophytosis
… The Takeaways
Key pearls to put into practice:
Dermatophytosis affects adoptable populations of animals, primarily puppies and kittens. The infectious nature of this condition is troublesome for shelters; some elect to “recognize and euthanize” to keep disease transmission to a minimum. There have, however, been several successful dermatophyte treatment programs developed in animal shelters, many of which use foster care families to aid in treatment delivery. By incorporating multimodal therapy (ie, combination of oral and topical antifungal therapy) with routine cleaning and disinfection, it is possible to eliminate environmental contamination and thereby reduce risk for reinfection and contagion.
Dermatophytosis is considered to be a generalized infection in cats due to the increased amount of infective material (ie, infective spores) present and distributed over the body as part of normal grooming behavior. This is different than in dogs, in which infection may be resolved with localized topical therapy. For cats, a combination of topical (eg, lime sulfur dips, miconazole/chlorhexidine combination shampoos) and systemic (eg, itraconazole, terbinafine) therapy is typically recommended.1
For most cats with alopecia, dermatophytosis should be considered a possible differential diagnosis. Positive Wood’s lamp fluorescence results will only be seen with Microsporum canis infections; a negative result does not rule out infection. Fungal culture remains the preferred diagnostic method to confirm disease, although dermatophyte PCR can also provide a rapid result to help confirm clinical suspicion.
You are reading 2-Minute Takeaways, a research summary resource proudly presented by Clinician’s Brief. Clinician’s Brief does not conduct primary research.