This response is incorrect. See below for the correct answer.
Enteral & Parenteral Nutrition in the Intensive Care Unit
Daniel L. Chan, DVM, DACVECC, DECVECC, DACVIM (Nutrition), DACVN, MRCVS, University of London, North Mymms, Hertfordshire, United Kingdom

Nutritional support is essential for critically ill patients in the intensive care unit and should be included as part of the standard of care, as there are potentially serious consequences of malnutrition. Effective nutritional management strategies can alleviate the risk for development of malnutrition and associated morbidities.1,2
Inadequate food intake, GI dysfunction, and metabolic changes can cause malnourishment in hospitalized patients not supported with nutritional interventions. Critically ill patients catabolize lean body mass during periods of food and nutrient deprivation, emphasizing the need for nutritional support2; this is also the case in obese patients, as critically ill patients with inadequate food intake preserve fat stores but catabolize lean body tissue.2 Cats do not downregulate gluconeogenesis or proteolysis during low protein intake.3 Continued loss of lean body mass can result in negative effects on wound healing, immune function, and, ultimately, clinical outcomes.2,4 Conversely, adequate energy substrates, protein, essential fatty acids, and micronutrients support wound healing and tissue repair.
Nutritional Assessment
Nutritional support carries a risk for complications (eg, hyperglycemia, electrolyte shifts, aspiration pneumonia), but these can be minimized through careful patient selection, nutritional assessment, and sound nutritional planning. A nutritional assessment should be performed through systematic evaluation to identify patients that require immediate nutritional support.5 Patients with obvious signs of malnutrition, >10% body weight loss, ≥3 days poor food intake, and prolonged illness should be given urgent nutritional support.5
Cardiovascular status should be stable and electrolyte, fluid, and acid-base abnormalities should be corrected before nutritional support is provided.
Nutritional Plan
A nutritional plan should include the anticipated duration of nutritional support, which largely depends on clinical judgment. The best route of nutrition (enteral or parenteral) should be determined, with the enteral route considered first when possible. If enteral feedings are not tolerated (when part or all of the GI tract is not functional [eg, with motility disorders]), parenteral nutrition can be considered so the patient is not without nutrition for >3 days. Nutrition should be introduced gradually, and target levels should be reached in 48 to 72 hours, except in patients at risk for refeeding syndrome.
Calculating Energy Needs
Resting energy requirement (RER) is the number of calories required to maintain homeostasis while the patient is at rest.2,4 RER is calculated as 70 × body weight in kg<sup0.75sup>. In patients that weigh 4.4 to 66 lb (2-30 kg), 30 × body weight in kg + 70 can be used to approximate energy needs. RER has historically been multiplied by an illness factor between 1.1 to 2 to account for increases in metabolism associated with different conditions and injuries. Recently, less emphasis has been placed on these subjective illness factors, and current recommendations include using RER as a starting point and adjusting based on the response to feeding.6
Although definitive studies determining the precise nutritional requirements for critically ill patients have not been performed, some recommendations are available. It is generally accepted that hospitalized dogs should be supported with 4 to 6 g of protein/100 kcal (15%-25% of total energy requirements) and cats should be supported with ≥6 g of protein/100 kcal (25%-35% of total energy requirements).5,7 Patients with poor protein tolerance (eg, those with hepatic encephalopathy) should receive reduced amounts of protein (dogs, ≈3 g/100 kcal; cats, 4 g/100 kcal).7 Patients with hyperglycemia or hyperlipidemia may also require decreased amounts of carbohydrates and lipids, respectively, when provided with parenteral nutrition.
Enteral Nutrition
Enteral nutrition is usually preferable, as it helps maintain GI structure and function. Nasoesophageal/nasogastric, esophagostomy, and gastrostomy feeding tubes are commonly used in dogs and cats. Considerations for various feeding tubes should be reviewed (Table). Guidance on placement of feeding tubes is available (see Suggested Reading).
Most complications with feeding tubes include tube occlusion and localized irritation at the tube exit site.8,9 More serious complications include infection at the exit site or, rarely, complete tube dislodgment and peritonitis with a gastrotomy tube (proper stoma require 10 days to form). Risk for complications can be reduced by using the appropriate tube, through proper food selection and preparation, and with careful monitoring.8,9
Feedings are generally administered every 4 to 6 hours, and feeding tubes should be flushed with 5 to 10 mL (based on size of patient and tube) of water before and after each feeding to minimize obstruction of the tube. At discharge, the number of feedings should be reduced to 3 to 4 times per day to help facilitate pet owner compliance.
A volume of 5 to 10 mL/kg per individual feeding is generally well-tolerated but can vary by patient. Enteral diets are mostly composed of water (most canned foods are already >75% water); thus, the amounts of fluids administered parenterally (including water from pre- and postfeeding flushes) should be adjusted to avoid volume overload. Premature removal of tubes can be prevented by using special collars (eg, Elizabethan) and wrapping the tube securely. Care should be taken to avoid tightly wrapping the tube, as this could lead to patient discomfort and even compromise proper ventilation.
CONSIDERATION FOR DIFFERENT TYPES OF FEEDING TUBES
Parenteral Nutrition
Indications for parenteral nutrition include persistent vomiting, severe malabsorptive disorders, and severe ileus. Safe administration of IV nutrition requires a dedicated catheter placed using an aseptic technique; this should only be provided by a 24/7 care facility where close monitoring can be provided.7 Long catheters composed of silicone, polyurethane, or tetrafluoroethylene are recommended for use with parenteral nutrition to reduce the risk for thrombophlebitis.7 Most parenteral nutrition solutions contain a carbohydrate (dextrose), protein (amino acids), and fat (lipids) source. The proportions of each component in the admixture are determined based on the required energy and protein needs of the patient. Detailed instructions for formulation of parenteral nutrition admixtures are available.7 Compounding parenteral nutrition admixtures requires special equipment and is commonly sourced from human hospitals. Alternatively, there are a few commercially available, ready-made, 3-in-1 solutions (Figure) that provide 40% to 70% of a patient’s RER (depending on the size of the patient) when administered at 2 to 4 mL/kg/hour; these solutions contain ≈20 mmol/L of potassium and therefore cannot be administered at higher rates.7 The osmolarity of these solutions can vary, but solutions of <600 to 750 mOsmol/L can be suitable for peripheral administration.7
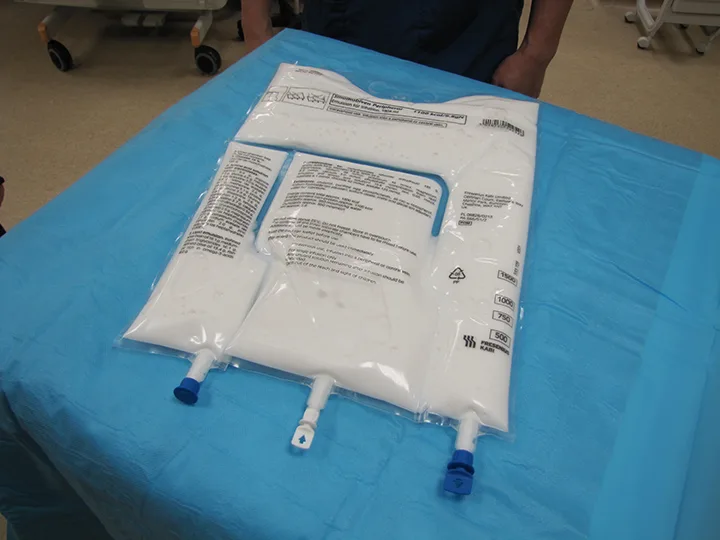
A commercially available, ready-made, 3-in-1 solution that contains dextrose, amino acids, and lipid emulsion can be used as an alternative to compounding parenteral nutrition with specialized equipment. The solution can be mixed just prior to use by squeezing the bag.
Monitoring & Reassessment
Daily monitoring of body weight in patients supported with nutritional interventions is recommended. However, fluid shifts should be accounted for when changes in body weight are evaluated; thus, BCS assessment is also important. Using RER as the patient's caloric requirement as a starting point, the number of calories provided may need to be increased (typically by 25% if well-tolerated) to meet the patient's changing needs. In patients unable to tolerate prescribed amounts, reducing amounts of enteral feedings and supplementing feed with parenteral nutrition should be considered.
Possible complications of parenteral nutrition include thrombophlebitis and metabolic disturbances (eg, hyperglycemia, electrolyte shifts, hypertriglyceridemia). Avoiding serious complications associated with parenteral nutrition requires early identification of problems and prompt action. Frequent monitoring of vital signs, catheter exit sites, and routine serum chemistry profiles can help identify developing problems. Persistent hyperglycemia while the patient is receiving nutritional support may require adjustment to the nutritional plan (eg, decreasing dextrose content in parenteral nutrition) or administration of regular, short-acting insulin.
Continual reassessment can help determine when to transition the patient from assisted feeding to voluntary consumption of food. Nutritional support should only be discontinued when the patient can consume ≈75% of their RER without support. In patients receiving parenteral nutrition, the transition to enteral nutrition should occur over at least 12 to 24 hours, depending on tolerance of enteral nutrition.