Emergency Management of Spinal Cord Lesions
Trauma, infarct, disk rupture, tumor, and infection are just a few causes of spinal cord damage. Regardless of pathology, however, the effect of spinal cord injuries can be quite devastating, even when managed appropriately.
StabilizationAnimals with suspected acute spinal injury should be transported on a flat surface to prevent movement or pressure on the spine. When a high cervical lesion or head injury is anticipated, head and neck movement must be avoided to prevent brain herniation or damage to the cord from a dens (odontoid) fracture (see Analgesia & Additional Stabilization, page 30).
Diagnosis & AssessmentClinical SignsThe patient may present with excruciating pain and weakness but have very mild disk protrusion with little spinal cord damage. Alternatively, animals presenting with mild pain may actually have significant loss of motor function as a result of excessive disk material causing substantial compression of the spinal cord.
Physical ExaminationThe clinician must first determine the severity of the spinal cord lesion; then localize the lesion to within 1 or 2 spinal cord segments. These determinations are initially made by neurologic examination (Figures 1 and 2).
Acute spinal cord pathology that suggests a severe lesion warrants timely advanced diagnostics and often surgical decompression. The following neurologic findings are used to assess the severity of the cord injury and where the lesion is located within the spinal cord.
Figure 1: This schematic is a cross section of the spinal cord between cervical cord segments 1 and 5. The clinical signs associated with disruption of a spinal tract’s activity are provided with the spinal tract’s name.
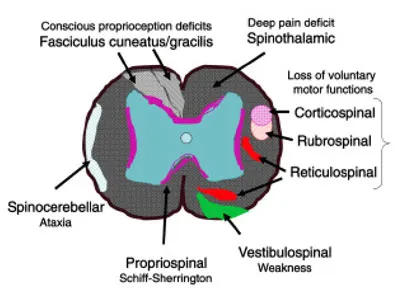
How Severe Is the Lesion? (Figure 1) Back PainBack pain is a consequence of irritation or inflammation of the membranes (meninges) surrounding the spinal cord, which contain a high number of pain fibers. Problems, such as mild ventral disk protrusion, can cause significant pain with subtle or no motor abnormalities depending on the degree of cord compression. When paresis or paralysis and severe back pain are present, hemorrhage or inflammation around the cord should be suspected. In these animals, back pain can ascend and/or descend from the original site of injury, suggesting a serious complication.
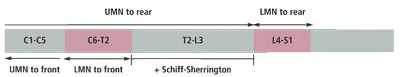
Figure 2: The gray rectangle represents the spinal cord. The lumbosacral intumescence lies between spinal cord segments L4 to S1, and the cervical intumescence lies between spinal cord segments C6 to T2. By drawing a vertical line through the spinal cord at the level of the lesion, the line will intersect the reflex changes anticipated in the limbs.
(C = cervical; L = lumbar; LMN = lower motor neuron; S = sacral; T = thoracic; UMN = upper motor neuron)
AtaxiaThe cerebellum controls coordination of the limbs. Ataxia resulting from a spinal cord lesion is a consequence of interference with the spinocerebellar tract located in the superficial, lateral edge of the spinal cord white matter. Vestibular disease can also cause ataxia; however, it is accompanied by additional neurologic abnormalities associated with the vestibular apparatus, such as head tilt, nystagmus, and rolling.
Extensor ToneWith the animal standing, pushing down over the spine at the level of the rearlimbs and the forelimbs will determine extensor tone of the limbs. The normal animal will resist the downward push by using its limbs to work against the pressure. Loss of extensor tract input results in weakness (paresis) that prevents resistance of pressure.
Dogs and cats have 2 major extensor tracts: the vestibulospinal tract and reticulospinal tract. The vestibulospinal tract is located superficially on the ventral aspect of the spinal cord white matter and is initially compromised with mild ventral cord pathology.
LMN = lower motor neuron; UMN = upper motor neuron
Conscious ProprioceptionThis is a response, not a reflex. The test is performed by turning over the foot so that the animal’s body weight is resting on the dorsal surface of the foot. Sensory input from the abnormally placed foot is sent through spinal tracts (fasciculus cuneatus for the forelimbs; fasciculus gracilis for the hindlimbs) in the dorsal columns of the cord.
These ascending tracts synapse at their respective nuclei in the brainstem and then travel through the thalamus to the cerebral cortex. The cortex then directs the voluntary movement through the cerebellum and flexor and extensor tracts to correct the foot position. Loss of conscious proprioception resulting from a spinal cord lesion indicates dorsal cord compression or malfunction and, in some cases, loss of voluntary motor movement.
Voluntary Motor ActivityLoss of voluntary motor activity (paralysis) due to a spinal cord lesion implies cord pathology deep within the white matter, typically involving the flexor and extensor tracts. Many of these tracts are located in the ventral and deep lateral cord spaces.
Voluntary motor activity can be tested with a technique known as tail-walking. While the clinician grasps the base of the tail and supports the animal’s body at the level of the affected limbs, the pet is encouraged to support weight and move the limbs. When the animal has voluntary motor activity, there is no need to check for deep pain perception.
Superficial & Deep PainSuperficial pain, or pain detected by pinching the skin, is carried by large nerve fibers distributed throughout the white matter of the spinal cord. In contrast, deep pain (ie, a dull, nonlocalized pain) is carried in the spinothalamic system, which is an ascending tract consisting of small neurons located diffusely throughout the white matter of the cord. This area is usually the last to be affected in spinal cord compression.
To test for deep pain, the clinician pinches the animal’s toes firmly or scrapes the periosteum of the toe with a sterile needle. For deep pain to be present, the animal must demonstrate conscious recognition of the pain (such as vocalization or a swift head turn in toward the stimulus) and not merely limb withdrawal. Absence of deep pain suggests that the lesion is severe, bilateral, and deep.
Schiff-Sherrington ReflexThe propriospinal (or fasciculus proprius) tract is located around the gray matter deep within the cord at segments T2 to L3. Inhibition and coordination of the frontlimbs occurs with respect to movement of the rearlimbs through this tract. With severe, deep, diffuse spinal cord compression between T2 and L3, this tract is compromised, resulting in severe extensor rigidity of the forelimbs and paralysis of the rearlimbs (called the Schiff-Sherrington reflex). With the exception of increased extensor tone, thoracic limb function is characteristically normal in this syndrome—distinguishing the injury from a C1 to C5 lesion.
Where Is the Lesion? (Figure 2)Reflex Arc
Any reflex or voluntary movement of the limbs requires that the lower motor neuron (LMN) reflex arcs are intact.
The rearlimb LMN reflex arc is located within spinal segments L4 to S1 (lumbosacral intumescence) and the forelimb arc from spinal segments C6 to T2 (cervical intumescence).
A lesion within any portion of the reflex arc results in slow or absent reflex activity in the corresponding limbs.
Slow or absent reflexes occurring in all 4 limbs implies a multifocal spinal cord lesion (C6–T2 and L4–S1) or peripheral disease (LMN, myoneural junction, or muscle).
Hyperreflexia
Coordinated limb movement occurs only through coordination of flexors and extensors by the cerebral cortex and cerebellum.
The neurons that regulate this movement, upper motor neurons (UMNs), arise in the brain and descend down the cord to the LMNs within the cervical and lumbosacral intumescence.
Damage to the UMNs results in exaggerated reflexes (hyperreflexia) due to the loss of coordinated activity from the higher centers; therefore, this finding suggests a lesion above the level of the intumescence.
Panniculus Reflex
The panniculus reflex is movement of the skin in response to pinching or pinprick. It can be tested from T2 to the caudal lumbar area.
Below the lesion, skin movement will be decreased or absent in response to pinching. When the panniculus response is present, quivering of the skin is seen due to reflex arc activity from the skin pinched to the cutaneous trunci muscle below the skin.
The reflex requires that the afferent stimulation travel up the spinal cord to T2, then out to the muscle and skin. The sensory nerve supplying a dermatome enters the spinal cord 1 to 2 vertebral bodies anterior to where the skin twitch occurred. For example, a skin twitch noted at spinal vertebral L1 to L2 level suggests that the lesion may be located at T12 to T13 or T13 to L1.
Before assigning the location of the lesion, the clinician must take into consideration both the information gathered from assessing the panniculus reflex and any reflex changes of the rearlimbs:
If the panniculus response occurs at T13 to L1 but the animal has no rearlimb reflex activity, the lesion is then diffuse or multifocal. Asymmetry of the panniculus reflex between the right and left is important and may result from cartilaginous infarct or lateralized disk material or hemorrhage.
Myelomalacia and hematomyelia are devastating complications of spinal cord injury and should be suspected whenever the localization of the lesion is expanding anterior or posterior to the original site. Fever, shock, and severe pain often accompany these findings.
It is not unusual for a cervical spinal lesion at or above the level of the cervical intumescence to result in normal reflexes but substantial neck pain. The vertebral space housing the cervical spinal cord is considerably larger than that containing the thoracic or lumbar spinal cord. Larger amounts of disk material or hemorrhage can occur here with minimal cord compression. However, irritation of the meninges and nerve roots located peripherally may cause severe neck pain and lifting of the frontlimb on the side of the lesion (called a root signature).
Analgesia & Additional Stabilization
After completing the initial neurologic examination, the patient should be sedated and given analgesics. Benzodiazepines will not alter the neurologic examination but may not provide the depth of analgesia obtained from opioids.
Whether the injury has been caused by trauma, hemorrhage, infection, or tumor, stabilization of concurrent systemic problems is critical. Results from an emergency database (including packed cell volume, total solids, blood glucose, blood urea nitrogen, electrolytes, lactate, and blood gases) guide the initial systemic stabilization (see Additional Diagnostics).
Shock, hemorrhage, pulmonary contusions or edema, and bone fractures can necessitate fluid resuscitation, oxygen therapy, hemostasis, and bandages.
With spinal trauma, a back brace to stabilize vertebral fractures or luxations may help avoid further damage from movement.
Additional Diagnostics
A complete blood count, serum biochemical profile, coagulation profile, and urinalysis should be performed; infectious disease titers may also be appropriate.
Blood pressure measurement, electrocardiography, and other diagnostics are performed as indicated by systemic findings.
Plain radiographs of the spine may rule out obvious spinal pathology, such as fractures, discospondylitis, collapsed disk spaces, or bone lysis. Ventrodorsal and lateral radiographs of the spinal column are necessary, possibly requiring a horizontal beam to avoid movement of the vertebra.
Advanced diagnostics include myelography, computed tomography, and magnetic resonance imaging of the spine.
MonitoringRepeated neurologic examinations form the basis for monitoring spinal cord pathology. Any progression of severity or change in localization of the lesion may warrant aggressive diagnostics or therapeutics. The respiratory rate and effort, as well as pulse oximetry, should be monitored in animals with high cervical lesions to anticipate brainstem swelling. Systemic problems are monitored as indicated.
TreatmentCage rest, analgesics, and sedation are the mainstays of therapy for mild signs of spinal cord pathology (eg, pain, ataxia, weakness). More aggressive monitoring and therapeutics become necessary when the animal demonstrates decreased voluntary motor activity.
MedicationsSteroids
High-dose steroid therapy with methylprednisolone sodium succinate (MPSS) has been recommended for acute traumatic cord lesions to reduce the effects of secondary injury (eg, swelling, inflammation), but no clinical studies have conclusively demonstrated efficacy.
One high-dose steroid regimen is as follows:
♦Initial administration: 30 mg/kg IV♦2 and 4 hours later: 12.5 mg/kg♦7 hours later: 2.5 mg/kg/hr for a total of 48 hours from the time of initial administration.
Clinicians electing to use this therapy should be aware, however, that case studies in dogs have shown that 33% to 90% of animals experience severe adverse effects, including diarrhea, vomiting, and other gastrointestinal signs, and the drug may also hinder neuronal regeneration.1
MPSS = methylprednisolone sodium succinate
MannitolIntravenous mannitol at 0.1 g/kg has been recommended for severe neurologic deficits when there is no evidence of active hemorrhage into the spinal column.2,3
SurgicalSurgical exploration, decompression, and spinal vertebral stabilization may offer the greatest likelihood for neurologic recovery.
Additional Treatment• Ongoing analgesia, weight control, special diets, acupuncture, and rehabilitation programs can promote return of neurologic function.• Research is also ongoing to determine the utility of polyethylene glycol to restore axonal integrity and reduce oxidative stress.
See Aids & Resources for references and suggested reading.