Ear Swabs: Technique & Interpretation
Patrick Hensel, DrMedVet, DACVD, University of Georgia
Otitis externa is one of the most common reasons dogs are presented to a veterinarian. Cytologic evaluations of ear swabs are crucial for assessment and management of recurrent ear infections.
Technique
Cytologic examination of ear swabs is a simple and quick in-house method to microscopically assess a patient's ears. Samples for cytologic examination are obtained by gently inserting cotton swabs into the horizontal ear canal. The swab is then rolled onto a microscopic slide until the specimen is evenly distributed (Figure 1).
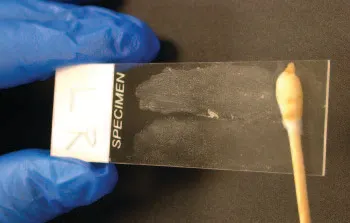
Preparation of ear cytology—rolling a cotton swab evenly over a microscope slide
For simple and fast staining, modified Wright's stain (Diff-Quik; diagnostics.siemens.com) is used. In order to reliably evaluate microorganisms, 5 to 10 HPFs (magnification, 100×; with immersion oil) should be assessed and findings averaged and recorded.
When ectoparasites are suspected, suspicious material should be placed, with a few drops of mineral oil, on a microscopic slide, followed by a coverslip. Mites can be easily detected at low magnifications (4× or 10×).
When should ear cytology be performed?
Ear cytology should be done for every patient with nonresponsive or recurrent otitis. It should also be performed at each follow-up examination to help evaluate the response to therapy, adjust treatment if necessary, and determine when therapy can be stopped. Depending on duration of therapy, cytology should be repeated every 2 to 4 weeks until otitis is resolved.
What information can be obtained from microscopic examination of ear swabs?
Microscopic examination is an effective method for semiquantitative evaluation of bacteria, yeast, parasites, and presence of inflammatory cells. It is not unusual for a patient to present with a mixed bacterial and yeast infection. The following factors should be considered when evaluating ear cytology:
Bacteria: The most common bacteria found in ears are cocci (Staphylococcus, Streptococcus) and rods (Pseudomonas, Proteus). These bacteria are approximately 0.5 to 1.5 mcm in diameter (Figure 2).
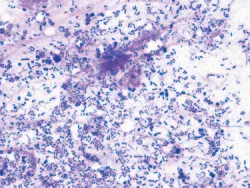
Cocci and rods too numerous to count (modified Wright’s stain; original magnification, 100´; immersion oil)
Yeast: Malassezia pachydermatis is the most common budding organism found in canine ears. This yeast is typically peanut-shaped, with a size ranging from 3 to 5 mcm. These organisms are often clustered around keratinocytes (Figure 3).
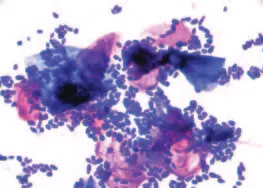
Malassezia yeast organisms (too numerous to count) clustered around keratinocytes (modified Wright’s stain; original magnification, 100´; immersion oil).
Cells: An occasional keratinocyte is to be expected, but in high numbers they may indicate seborrhea. Neutrophils with intracellular bacteria are typical in active ear infections with severe inflammation (Figure 4).
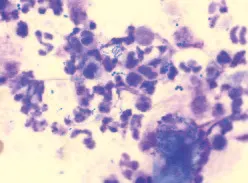
Multiple clusters of cocci and high numbers of neutrophils (modified Wright’s stain, original magnification, 100´; immersion oil)
Ectoparasites: The most common parasite, usually found in dark-brown crumbly discharge within the ear canal (especially in cats), is the ear mite Otodectes cynotis (Figure 5). Demodex mites may also be seen on ear smears (Figure 6).
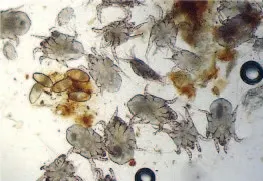
Multiple ear mites and cluster of 5 mite eggs (mineral oil; original magnification, 4´)

Two adult Demodex mites (mineral oil; original magnification, 10´)
When are cytologic findings clinically relevant?
Cocci and yeast belong, to some degree, in the normal microbiological skin flora. There is no absolute number, which can make it difficult to determine whether findings are normal or abnormal. Thus, in every case the importance of the microscopic findings should be determined in conjunction with other clinical signs (eg, inflammation, head shaking, scratching). Even low numbers of organisms, such as 1 to 5 cocci or Malassezia species per HPF, are considered relevant if the ears are bothering the animal. Presence of bacterial rods (eg, Pseudomonas spp) should always be considered pathogenic.
Why is ear cytology more reliable than bacterial and fungal culture?
Culturing allows identification of an organism and provides its sensitivity, which is important if systemic therapy is considered in patients with otitis media. However, culture and susceptibility results must be interpreted very carefully because differences between laboratories are common, growth of nonpathogenic bacteria can be observed, and Malassezia yeast may fail to grow on lipid-poor culture media. In addition, it is not unusual that findings on cytology do not correlate with culture results.
Because most patients with otitis externa can be managed successfully with topical therapy only, culture and susceptibility testing may not be necessary. Susceptibility of bacteria depends on drug concentration; since a much higher local concentration is achieved with topical therapy, such test results may not be clinically relevant. For this reason, in my opinion ear cytology more accurately reflects the true microbial population within the ear canal.
How should cytologic findings be recorded?
Ear cytology should be repeated at each follow-up examination. A standardized method does not exist, but the approach in the Table may be helpful. The same scale can be applied to recording inflammatory cells. A numeric scale may be more objective and minimizes interobserver variations, especially if a patient is seen by a different doctor at each visit.