Diagnosing Feline Respiratory Disease
Janice A. Dye, DVM, MS, PhD, DACVIM (SAIM)

Profile
Respiratory diseases are common in cats. This article will review how clinical signs and changes in breathing pattern provide important clues to the underlying functional deficits and disease processes present. With these clues, one can readily formulate a list of probable differential diagnoses that will guide the initial diagnostic approach and case management.
Signalment
Siamese breed is overrepresented in bronchial disease.
Probability of viral or parasitic causes increases in young or outdoor cats.
Outdoor cats are at risk for trauma or bite wounds (eg, pyothorax).
Incidence of neoplasia increases in older cats.
Causes
Major categories of feline respiratory disease include the following:
Infectious: Rhinitis, tracheobronchitis, and pneumonia due to viral, bacterial, protozoal (eg, toxoplasma), or fungal organisms
Parasitic: Direct effects or those secondary to immune responses to migrating larval or dead parasites
Inflammatory: Chronic bronchial disease, allergic bronchitis, inflammatory airway disease (ie, "feline asthma"), chronic bronchitis, chronic obstructive pulmonary disease, and interstitial lung diseases
Congenital or acquired conditions: Brachycephalic syndrome (in Persian cats), tracheal stenosis, ciliary dysfunction, pleural bullae, diaphragmatic hernia, mucosal or systemic (eg, FIV) immunodeficiency (clinical signs may not occur until later in life as secondary changes [eg, airway remodeling, bronchiectasis] develop)
Neoplastic: Primary nasal, laryngeal, tracheal, and pulmonary; also metastatic disease or compression by enlarged lymph nodes, thymus, or heart-base tumor
Cardiovascular: Cardiomyopathy/heart failure with pulmonary edema, pulmonary hypertension, pulmonary embolism
Injury-related: Airway or parenchymal damage due to inhalation of irritants (cigarette smoke, smoke inhalation from fire) or aspiration of foreign material (plant awn, food, gastric acid); comorbidity with laryngeal paralysis or megaesophagus
Signs & Pathophysiology
Altered Reflexes
The most common (most easily recognized) respiratory signs are sneezing and coughing.
Cats presenting for occasional cough, sneeze, or "weird sound from the throat" may well be healthy, and a cautious wait-and-see approach may be indicated.
Severe or persistent bouts of sneezing or coughing-particularly if cough occurs with wheeze-indicate significant irritation/inflammation of the nasal and lower air passageways, respectively.
Acute onset of sneezing with nasal or ocular discharge characterizes viral infection because the common feline agents (feline herpesvirus-1, feline calicivirus) are cytopathic to epithelial cells of the upper respiratory tract. Chronically, cats with upper respiratory disease seemingly lose their sneeze reflex; thus, nasal congestion becomes the predominant condition.
Cats have a particularly well-developed cough and gag reflex. Tracheobronchial cough can be stimulated by lower airway inflammation, excess production or retention of mucous secretions, irritation or pressure within or outside the trachea, and development of significant bronchoconstriction.
Posttussively, gagging or excessive swallowing may occur as the cat attempts to clear thickened expectorated mucus from the pharynx (Figure 1). In turn, pharyngolaryngeal cough may be induced. Owners frequently misinterpret the combination of coughing and gagging as evidence of "hair balls."

FIGURE 1 A Siamese cat with increased swallowing efforts after a bout of coughing.
Cough is a common sign in "asthmatic" cats; however, some cats with severe airway disease develop overt dyspnea, often with expiratory wheeze, but do not exhibit cough.
Altered Ventilation
Any process or condition that compromises a cat's ability to move air into and out of the lungs (ie, ventilate) and effectively exchange gas at the alveolar surface will result in changes in its breathing pattern, rate, and level of effort.
Subtle or intermittent changes can go unrecognized for prolonged periods.
It is essential to maintain patency of all the ductwork (ie, air passageways from the nares to the smallest bronchiolar ducts) (Figure 2A).
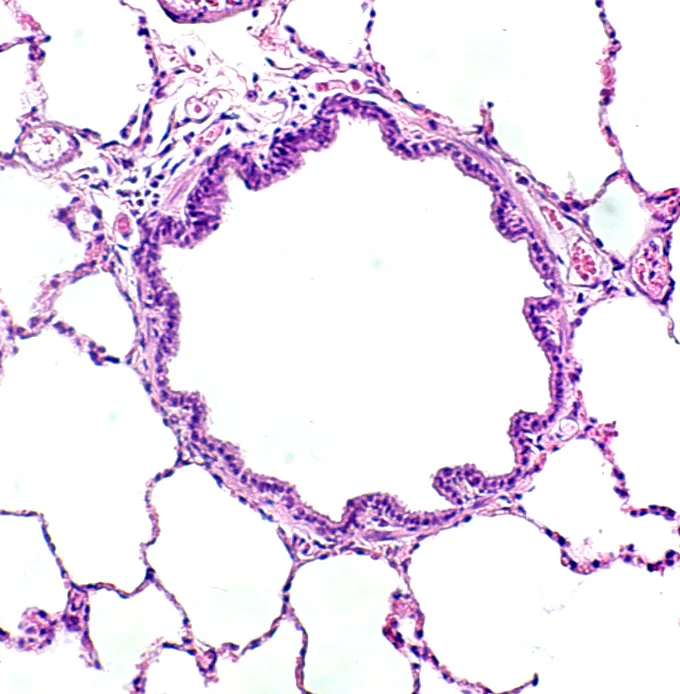
FIGURE 2 A patent airway in a healthy cat (A). An occluded airway from a cat with chronic disease (B). Intraluminal mucus and debris, smooth muscle thickening, numerous inflammatory cells and goblet cells, and subbasement membrane thickening are evident.
Normal ventilation requires a patent ductwork and functioning air pump. Any clogging, bending, or excessive narrowing of ductwork will substantially reduce airflow into (and out of) the lungs, leading to an obstructive type of breathing pattern.
Upper airway obstruction results in stertorous breathing (increased inspiratory noise and effort), often with prolonged inspiratory time (relative to expiratory time). Moreover, stertor is associated with changes to the proximal upper airways, whereas stridor originates in the laryngeal region, and snore in the palatal area.
Conversely, cats with "asthma" exhibit increased expiratory effort because of decreased patency of their small lower airways. This is a result of airway abnormality and the normal dynamic narrowing of small airways during expiration. "Asthmatic" cats have hyperreactive airways and are prone to developing spasm or constriction of airway smooth muscle.
Pathologic changes include airway mucosal changes (epithelial denudation, increased inflammatory cells) and increased goblet cells with intraluminal mucus and inflammatory debris. Substantial subbasement membrane thickening occurs with long-standing disease (ie, airway remodeling) (Figure 2B).
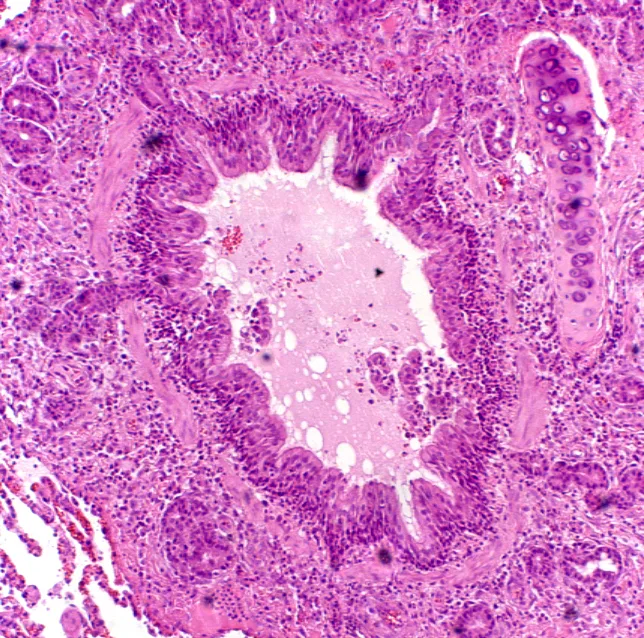
FIGURE 2 A patent airway in a healthy cat (A). An occluded airway from a cat with chronic disease (B). Intraluminal mucus and debris, smooth muscle thickening, numerous inflammatory cells and goblet cells, and subbasement membrane thickening are evident.
Accordingly, if and when significant airway obstruction develops, cats become dyspneic and possibly cyanotic, but not necessarily tachypneic.
A normal to reduced respiratory rate interval allows for more thorough exhalation. In other words, by dedicating a disproportionate time for expiration within each breath, the cat optimizes the amount of time that trapped "spent" air can exit through the narrowed ductwork.
Visually, one may observe end-expiratory abdominal pushes; on auscultation, end-expiratory wheezes are often detected.
Air pump failure results in a restrictive type of breathing pattern. Cats cannot take deep breaths. Restrictive disease can arise because of alterations in the lung parenchyma (eg, pulmonary fibrosis), pleural space (eg, effusion or air), chest wall (eg, rib fracture), or neuromuscular apparatus (eg, diaphragm fatigue).
Even if the ductwork is in perfect order, dysfunction of the air pump or bellows means that the cat cannot adequately expand its thoracic cavity (and, with it, the lungs). Thus, it has limited capacity to generate the bulk airflow required to provide oxygen-rich air to the deep lung. Cats compensate by increasing the frequency of their tiny breaths and reducing their activity.
Up to a point, these cats will not appear dyspneic per se, but they will probably remain tachypneic-even at rest. As such, they can quickly decompensate if oxygen demand increases (eg, from the stress of being examined or restrained). The astute veterinarian will pace the workup to allow the cat to "catch its breath" in between examination and diagnostic procedures.
Diagnosis
Feline respiratory disease has many known causes; however, the most common syndromes are idiopathic and thus diagnoses of exclusion.
Differential Diagnoses
Upper respiratory signs (sneezing, stertorous breathing, nasal discharge) commonly occur with acute viral infection or chronic (idiopathic) rhinosinusitis. Less common conditions include nasal neoplasia, fungal rhinitis, periodontal disease, foreign body, and nasopharyngeal polyps or webbing.
Coughing is common in cats with "asthma," occurs with varying frequency in cats with pleural space or parenchymal disorders (eg, pulmonary fibrosis), and seldom is seen in cats with cardiac disease. Hence, cats with cough, especially those with expiratory wheeze, should be evaluated for lower airway disorders.
Persistent tachypnea indicates restrictive lung disease. Idiopathic pulmonary fibrosis, a recently recognized disease in cats, is an important cause. Other conditions include parenchymal infiltration (eg, pulmonary edema), mediastinal changes (eg, thymic lymphoma), and pleural space disease.
Open-mouthed breathing with reduced breath sounds is an ominous combination due to severe, generalized bronchoconstriction or bilateral pleural space disease. In the former situation, cats are often cyanotic and may have sinus bradycardia.
Cardiac disease should always be considered in cats presenting with lethargy and tachypnea but no history of cough. Careful cardiac auscultation may detect murmurs or arrhythmias that guide the diagnostic workup (electrocardiography and echocardiography). Right-sided heart changes with tachypnea may indicate pulmonary hypertension.
Concurrent respiratory and gastrointestinal signs may indicate underlying parasites. Larval heartworm migration has been recently reportedly to induce pulmonary arteriolar abnormality with resultant cough, dyspnea, vomiting, and weight loss (ie, heartworm-associated respiratory disease).
Alternatively, cough with signs of rhinitis, gastroenteritis, or dermatitis may indicate underlying atopy (food or inhalant hypersensitivity).
Finally, it is not uncommon for cats to present in overt respiratory distress despite no known history of respiratory disease. Any cat presenting with tachypnea or dyspnea or respiratory signs in conjunction with illness (eg, fever or weight loss) should first be stabilized and then evaluated without delay.
Laboratory Findings/Imaging
Diagnosis of respiratory disease can be achieved only if one looks for specific causes. Because the common syndromes in cats are idiopathic, what you do not find can be as important as what you do find.
Several fecal analyses (Baermann preparations, flotation, sedimentation) are needed to detect certain pulmonary parasites (ascarids; Aelurostrongylus, Capillaria, and Paragonimus species).
Occult heartworm testing to detect antigens (from adult female or dying male worms) or antibodies (to current or previous infection) should be performed.
For chronic upper respiratory tract disease, evaluation often includes skull or dental radiography (or cranial computed tomography where available) in combination with a thorough orodental exam, rhinoscopy, and laryngoscopy.
Suspected pleural space disease can be further documented with thoracic radiography, ultrasonography, or diagnostic thoracocentesis. Pleural fluid evaluation is used to differentiate types of effusion (eg, chylothorax, effusive form of feline infectious peritonitis).
When lower airway tract disease is suspected, good-quality thoracic radiography is essential. Both lateral views and a ventrodorsal (or dorsoventral) view should be obtained. Radiography can confirm and localize disease and also provide information on severity of changes.
Radiographic changes in "asthmatic" cats often include a prominent bronchial pattern (tram lines and donuts) or a mixed pattern of bronchial, alveolar, or interstitial changes. With increasing disease severity or chronicity, atelectasisof the right middle lung lobe or left cranial lobe (caudal segment) and generalized lung overinflation may be evident (Figure 3).

FIGURE 3 Thoracic radiograph of a cat with long-standing disease. A prominent bronchial pattern, general hyperinflation, and atelectasis of the left cranial lobe (caudal segment) are evident.
Airway sampling and cytology (performed via tracheal wash or lavage, brushing, or bronchoscopy) are used to assess the presence of increased mucus (Figure 4A) and to characterize the type of inflammatory processes present (eg, predominantly eosinophilic or neutrophilic [Figure 4B]).
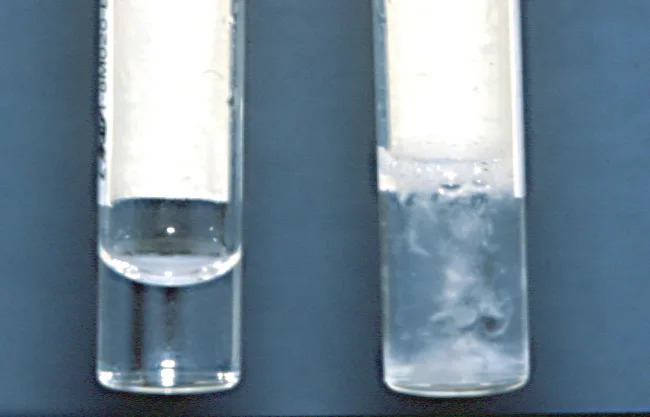
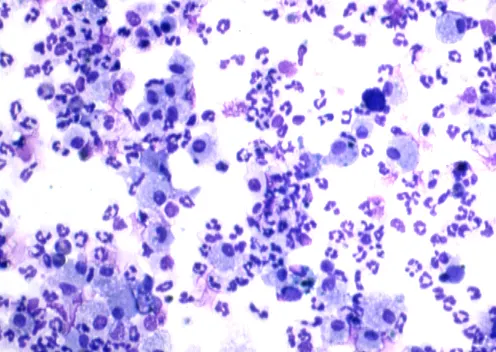
FIGURE 4 Airway lavage sample. Minimal secretions (left) versus thick strands of mucus (right) (A) and many nondegenerative neutrophils (B; original magnification, 20×). (Wright’s-Giemsa stain)
On occasion, neoplastic cells (eg, lymphoma) or organisms (eg, Toxoplasma gondii, Blastomyces dermatitidis) can be detected in specimens.
Positive bacterial airway cultures occur in approximately one third of cats with bronchial disease; however, it can be difficult to determine whether isolation of small numbers of bacteria reflects contamination or true infection.
If radiographs fail to reveal airway changes and instead reveal focal or nodular disease, lung aspiration (blind or ultrasonography-guided) may yield a diagnostic sample.
Increasingly, molecular testing (PCR, multiplex PCR strategies) used in conjunction with routine virus isolation or microbiologic assessment is improving our understanding of the significance of emerging or difficult to isolate organisms (eg, MRSA, feline herpesvirus or calicivirus, Bordetella bronchiseptica, Chlamydophila felis). Only reputable laboratories using validated protocols and other controls should be used.
Treatment
Medical
Depending on results, specific antimicrobial, antiparasitic, antifungal, or antineoplastic therapy may be indicated.
As with humans with asthma, cats with inflammatory airway disease may respond dramatically to a combination of bronchodilators (eg, methylxanthines, β2-adrenergics) and corticosteroids (either oral or inhaled).
Cats with chronic bronchitis/chronic obstructive pulmonary disease may also improve, albeit less dramatically, after receiving long-term combination corticosteroid and bronchodilator therapy.
Many nonspecific therapies, such as fluids, nutritional strategies, and antiinflammatory agents, can be beneficial, but further treatment discussion is beyond the scope of this article.
Client Education
It is important to discuss the most likely cause of the cat's signs, how diagnostic testing will help to rule in or out likely causes, and risks and benefits of certain less invasive versus more invasive diagnostic procedures.
Developing good client rapport is also essential because many feline respiratory syndromes are not curable and ultimately progress to cardiac or pulmonary insufficiency.
Follow-Up
Patient Monitoring
Treatment trials with follow-up examination and diagnostic testing are necessary to refine drug dosages and to effectively manage (although rarely cure) chronic respiratory disease in cats.
If the clinical signs are less clearly localizable or the signs worsen despite appropriate treatment, specialty referral may be warranted. For example, availability of cranial or thoracic computed tomography, fluoroscopy, or ultrasound-guide aspiration or biopsy may further assist in obtaining diagnostic samples or tissues.
Prevention
Adherence to vaccination schedules and limiting exposure to infectious agents (eg, boarding) are recommended.
Efforts to minimize exposure to irritants (dusty litter, cigarette smoke, noxious fumes), as well as allergens and molds (water damaged homes), are prudent and may prove beneficial as part of overall case management.