Cystocentesis (Step-by-Step Guide)
Philip Krawec, DVM, University of Tennessee
Adesola Odunayo, DVM, MS, DACVECC, University of Florida

Cystocentesis (ie, obtaining urine directly from the urinary bladder by inserting a needle through the body wall) is common and considered the ideal method for obtaining urine for urinalysis and culture and susceptibility testing.1 Cystocentesis typically helps prevent contamination (eg, from bacteria, RBCs, WBCs, or debris from the lower urinary tract and perineum) that can occur with voided or catheterized urine samples.2 Diagnosis of bacterial cystitis is somewhat simplified through cystocentesis, as samples through this method should be sterile3; quantitative bacterial counts should be analyzed when evaluating voided samples.4 Although frequently iatrogenic and self-limiting, hematuria may be noted in cystocentesis samples.5
The urinary bladder is located in the caudal abdomen and positioned within the pelvic inlet ventral to the colon. The urinary bladder may fall to the dependent portion of the caudal abdomen if the patient is in lateral recumbency. The ureters terminate in the dorsal aspect of the bladder at the trigone. The urinary bladder is primarily composed of striated muscle, and blood is supplied by cranial and caudal vesical arteries. When filled, the urinary bladder can be easily palpated in most patients; however, palpation may not be feasible in some obese patients or in patients with either a low volume of urine or anatomic abnormalities (eg, pelvic bladder).6
Indications for cystocentesis include collecting urine samples from patients for which a urine sample is needed. Most cystocentesis samples are used for urinalysis and urine culture and susceptibility testing. Other diagnostic tests may include urine protein:creatinine ratio, urine cortisol concentration, urine catecholamine concentration, urine leptospirosis PCR, and urine electrolyte concentration.
Cystocentesis may also be used therapeutically in patients that have urinary obstruction secondary to uroliths, urethral plugs, and/or neoplasia. Decompressive cystocentesis can alleviate patient discomfort prior to urinary obstruction removal and can lower intraluminal bladder pressure and facilitate retropulsion of urethral plugs/uroliths, potentially easing catheterization.7 Decompressive cystocentesis should be performed with an extension set and a 3-way stopcock to allow for a single needle insertion as opposed to multiple needle insertions. Although decompressive cystocentesis has previously been discouraged, studies have suggested there is minimal risk for bladder rupture/uroperitoneum.8
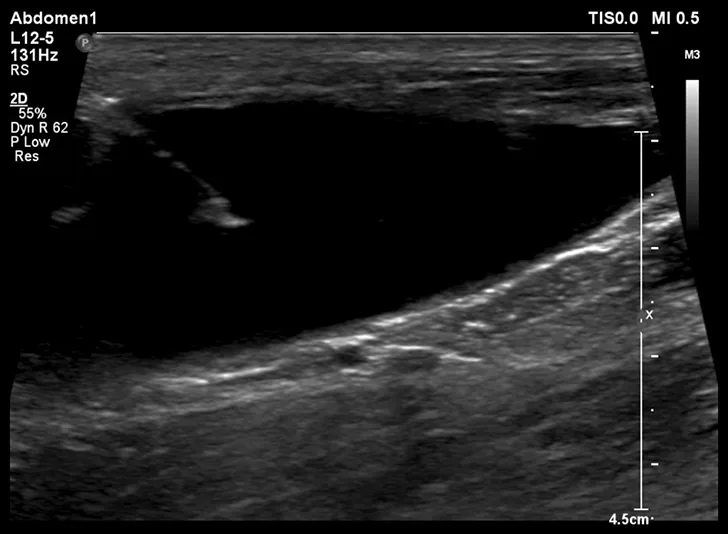
Cystocentesis is often performed with ultrasonographic guidance, although this is not required (ie, blind cystocentesis). Using ultrasonography can help direct visualization of the needle in the urinary bladder lumen, avoiding iatrogenic damage of surrounding structures (Figure 1). The relative size of the bladder, echogenicity of its contents, and any obvious structural abnormalities can also be observed. A primary advantage of blind cystocentesis is that it does not require special equipment. Cystocentesis can be challenging to perform in patients that have abdominal effusion and should be performed with ultrasonographic guidance in such cases.
Cystocentesis is usually performed in awake patients, but sedation should be considered in fractious or uncooperative patients. See Related Article for a full outline of a sedation protocol.
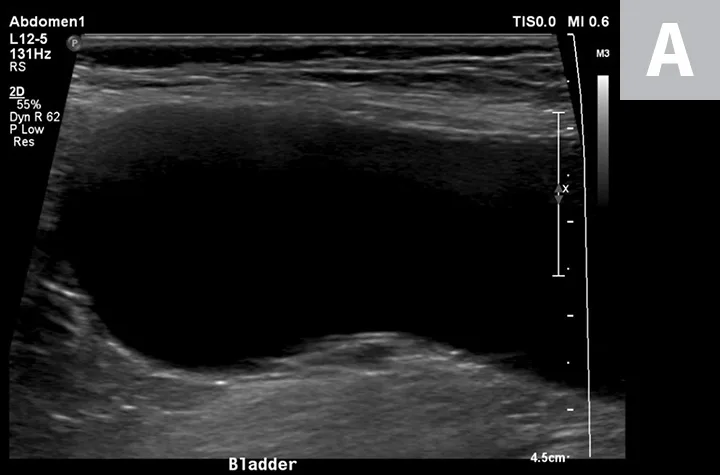
Ultrasonographic image showing the cranial aspect of the urinary bladder (A), identified just before ultrasound-guided cystocentesis. It is important to adjust the depth of the image so that the urinary bladder is focused and to consider the depth of the urinary bladder using a machine scale that should be present on the ultrasound screen; in smaller patients the needle may only be partially inserted and not reach the hub (B; arrow).
Considerations & Contraindications
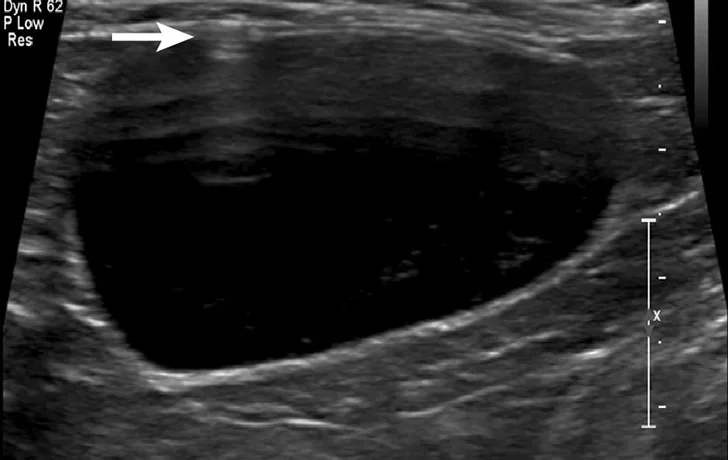
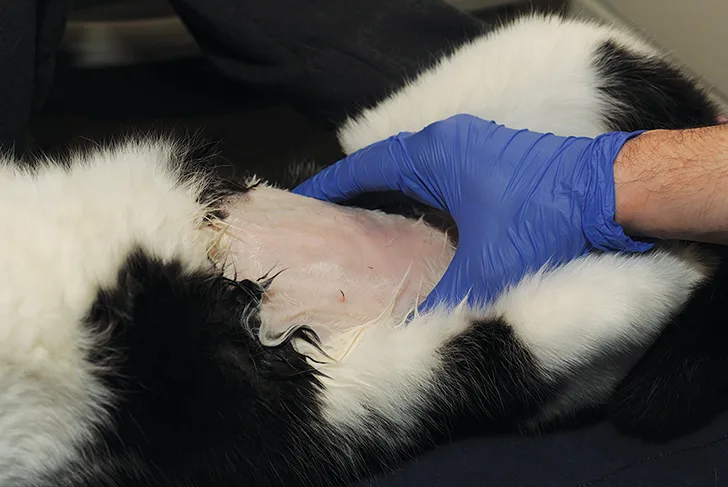
Blind cystocentesis is contraindicated in patients with reproductive disorders (eg, pyometra); use of ultrasonographic guidance is recommended for such patients. There are no specific contraindications to blind cystocentesis in male dogs, although blood vessels on either side of the prepuce should be avoided (Figure 2).

Blind cystocentesis in a male dog. The right caudal superficial epigastric veins (arrows) can be noted and should be avoided.
There are some conditions, however, in which cystocentesis should be avoided entirely. Cystocentesis should be avoided in patients with pyoderma to prevent possible introduction of bacteria into the abdominal cavity and in patients that are unstable, as putting unstable patients in dorsal or lateral recumbency may lead to decompensation of hemodynamic status. Cystocentesis is also contraindicated in patients that may have bladder neoplasia, as cystocentesis in these patients can increase the risk for seeding neoplastic cells into the abdominal cavity.9
Coagulation status (ie, prothrombin time, activated partial thromboplastin time, thromboelastography, platelet count) should be considered before performing cystocentesis in patients at risk for bleeding. In addition, laceration or perforation of intra-abdominal blood vessels (eg, aorta) can lead to life-threatening hemorrhage.10 Abdominal exploratory surgery may be required in patients that develop hemoabdomen or uroabdomen following cystocentesis that cannot be stabilized with conservative management.10,11
Other potential complications include bladder wall hematoma, bladder wall rupture leading to uroabdomen, intravesicular blood clots, focal peritonitis, peritoneal free gas, abdominal wall abscessation, nodular fat necrosis, aortic or bladder wall hematoma, and bladder mucosal detachment.12 Vasovagal collapse has also been reported in cats following cystocentesis.13 In addition, one case report describes a dog with bacterial cystitis that developed septic peritonitis following cystocentesis.11
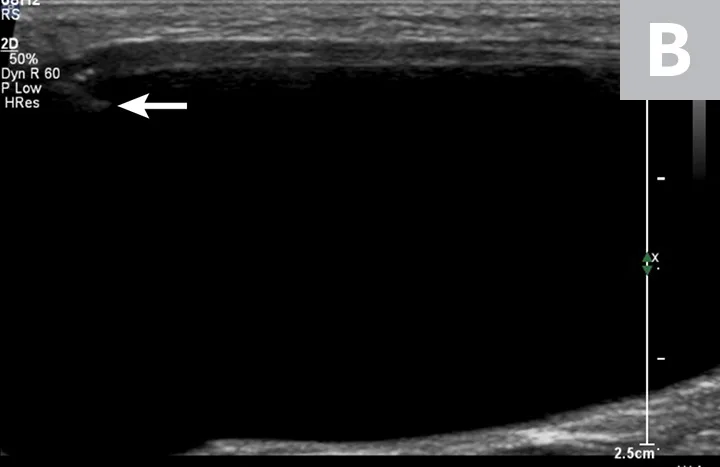
After cystocentesis, a small amount of gas may be introduced into the urinary bladder iatrogenically but is typically of no clinical consequence (Figure 3). Evidence of this can be seen on ultrasonography after the procedure is completed and appears as horizontally oriented, parallel hyperechoic lines reverberating off the introduced gas.
Reverberation artifact from free gas that was iatrogenically left in the urinary bladder after cystocentesis, noted by the parallel, horizontally oriented hyperechoic lines extending into the urinary bladder (arrow). This is not considered a complication but may be seen following the procedure.
Patient Preparation & Positioning
Depending on clinician preference and patient temperament, a staff member may hold the patient. Patients can be positioned in either dorsal or lateral recumbency. The authors prefer lateral recumbency in cats. In female dogs in dorsal recumbency, the bladder is usually located below the umbilicus, where isopropyl alcohol pools. A V-trough may help maintain patient comfort in dorsal recumbency. For patients in dorsal recumbency, the urinary bladder is often located on the midline between the fourth and fifth nipples. In male dogs, the prepuce makes aspiration of urine on the midline difficult. Paramedian insertion of the needle is acceptable; however, the caudal superficial epigastric veins that lie on either side of the prepuce should be avoided. Standing cystocentesis, which involves puncturing through the lateral abdominal wall, has been described as safe and effective and may be less stressful for patients.14
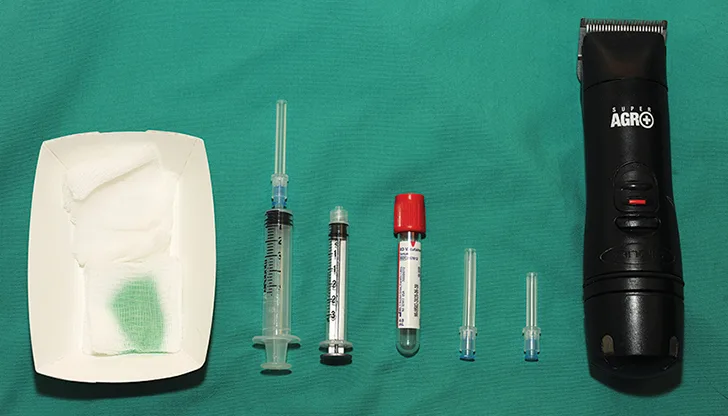
Although there are no evidence-based recommendations, the authors recommend preparing the ventral abdomen by clipping the hair and scrubbing the proposed insertion site to minimize the risk for iatrogenic bacterial peritonitis (Figure 4).

A restrained dog in dorsal recumbency for cystocentesis; the caudoventral abdomen has been clipped and scrubbed with an antiseptic solution.
What You Will Need
Clippers and antiseptic solution (dilute chlorhexidine or iodine-based preparation)
1- to 1.5-inch, 22-g needle
3- to 12-mL syringe
Collection tubes (glass red top tube or any empty tube without preservatives).
A nonadditive sterile tube is generally recommended for culture. There are other tubes available that may aid in keeping bacteria viable in transit. A reference laboratory can typically help identify appropriate tubes for urine-based tests.
Ultrasound machine (for ultrasound-guided cystocentesis only)
Sedating agent, if needed
70% isopropyl alcohol
Additional supplies if removing a large volume of urine
Extension set
Alternatively, a butterfly catheter can be used in smaller patients in lieu of an extension set and needle
3-way stopcock
Larger syringe (12-60 mL)
V-trough (optional)
Step-by-Step: Ultrasound-Guide Cystocentesis
General Author Insights
Avoid moving or repositioning the needle in the abdominal cavity. If urine is not obtained after the first aspiration, pull the needle straight out without repositioning to avoid laceration of any major structures. The needle should also be quickly removed if the patient is uncooperative. Use a new needle for each cystocentesis attempt.
If obvious blood is obtained during cystocentesis, stop aspiration and discontinue further attempts. Rule out significant hemorrhage by evaluating the patient's heart rate, blood pressure, respiratory rate, and mucous membrane color. This should be done immediately and at least every 15 minutes for the first hour. Peripheral packed cell volume/total solids should be evaluated in patients suspected of having significant hemorrhage. Evaluate the abdominal cavity immediately and again 15 minutes later, using ultrasonography to look for free abdominal fluid. Consider sampling the abdominal fluid if a mild to moderate amount of fluid is present to rule out uroabdomen or hemoabdomen.
If the urinary bladder is too small to obtain a sample, wait 30 to 120 minutes, then reassess the size of the urinary bladder. Administering fluids (IV or SC) may help increase urine volume, but certain results (eg, urine specific gravity) may be skewed.
Step 1
Place the patient in either dorsal or lateral recumbency. If the patient is a male dog, gently retract the penis off the midline.
Gently palpate the caudal abdomen to isolate and secure the urinary bladder.

Step 2
Using an ultrasound probe, visualize the urinary bladder. Insert the needle attached to a syringe roughly 5 to 10 mm cranial to the ultrasound probe. Introduce the needle at a 45° angle to the transducer probe and pass it into the abdomen in a cranial-to-caudal orientation.


Author Insights
Before inserting the needle, pull back on the syringe plunger and push it back into place (ie, pop the seal) to prevent marked movement of the needle tip resulting from increased resistance that occurs during the first pull back.
Avoid damaging the ultrasound transducer probe with the needle (Figure) during cystocentesis, as scratching its surface will decrease the lifespan of the probe and can affect image quality.

Step 3
Visualize the needle (appears as a hyperechoic line with distal shadowing [seen in the top left of the Figure]), then advance it into the urinary bladder lumen, terminating near the junction of the bladder and urethra (seen on the right side of the Figure).
Step 4
Apply negative pressure to the syringe to obtain the sample, then release the negative pressure and slowly withdraw the needle.

Author Insight
A repeat scan of the urinary bladder area, especially along the needle tract and just cranial to the apex of the bladder, can be performed to evaluate for evidence of a urine leak.
Step-by-Step: Blind Cystocentesis
Step 1
With the patient in either lateral or dorsal recumbency and a staff member holding the patient, gently palpate the caudal abdomen and isolate the urinary bladder.

Step 2
Using gentle digital pressure, secure the urinary bladder with one hand. If the patient is in dorsal recumbency (Figure), insert the needle with the syringe attached in a cranial-to-caudal orientation and a 45° angle to the body wall. If the patient is in lateral recumbency, insert the needle in a cranial-to-caudal orientation while approaching the urinary bladder from its lateral aspect.

Author Insight
Before inserting the needle, pull back on the syringe plunger and push it back into place (ie, pop the seal) to prevent marked movement of the needle tip resulting from increased resistance that occurs during the first pull back.
Step 3
Apply negative pressure to the syringe to obtain the sample, then release the negative pressure and slowly withdraw the needle.



Blind cystocentesis in a cat restrained in lateral recumbency (A). The urinary bladder is stabilized with one hand while the needle is inserted into the urinary bladder through the flank. Blind cystocentesis in a cat restrained in dorsal recumbency (B). The urinary bladder is stabilized with one hand while the needle is inserted into the urinary bladder along the ventral midline. Blind cystocentesis demonstrating paramedian needle insertion in a male dog (C). The caudal superficial epigastric veins (arrows) can be noted and should be avoided.
Related Article
For a full outline of a sedation protocol that can be used for cystocentesis, see Top 5 Short Procedure Sedation Scenarios.
The authors would like to thank Phil Snow and Dr. Kryssa Johnson for assistance in obtaining images, as well as Vibe Hespel and Penny Hedges for their support.
Images were simulated for illustrative purposes. Cystocentesis was not performed in the patients shown in this article.