
Indolent corneal ulcers (ie, spontaneous chronic corneal epithelial defects, boxer ulcers) are superficial ulcers with an abnormal and often prolonged (>5-7 days) healing process, typically due to a defective interaction between the basal corneal epithelium and basement membrane.1,2 These ulcers are commonly seen in boxers but have been reported in other canine breeds.3
Association With Patient Age
Indolent corneal ulcers are most common in patients ≥6 years of age and should be considered in middle-aged dogs with corneal erosion that has not healed in 1 to 2 weeks following topical antibiotic treatment. Underlying causes of delayed healing (eg, distichia, ectopic cilia, trichiasis, foreign body, infection, tear film abnormality, exposure, facial nerve paralysis) should be ruled out prior to diagnosis, particularly in dogs <6 years of age.1
Clinical Signs
Clinical appearance typically includes a ring of loose epithelium that results in a diffuse ring or halo of less intense fluorescein staining around the defect (ie, halo sign; Figure). Indolent corneal ulcers are superficial, have no stromal loss or evidence of infiltrate (indicating infection), are often present in the axial or paraxial cornea, and may be vascularized. Application of a topical anesthetic and cotton-tipped applicator debridement to loosen corneal epithelial tissue can aid in diagnosis if an indolent ulcer is suspected but not obvious on fluorescein stain. Patients often exhibit blepharospasm, conjunctival hyperemia, and epiphora, and pet owners may report the patient has been rubbing or pawing at the eye.
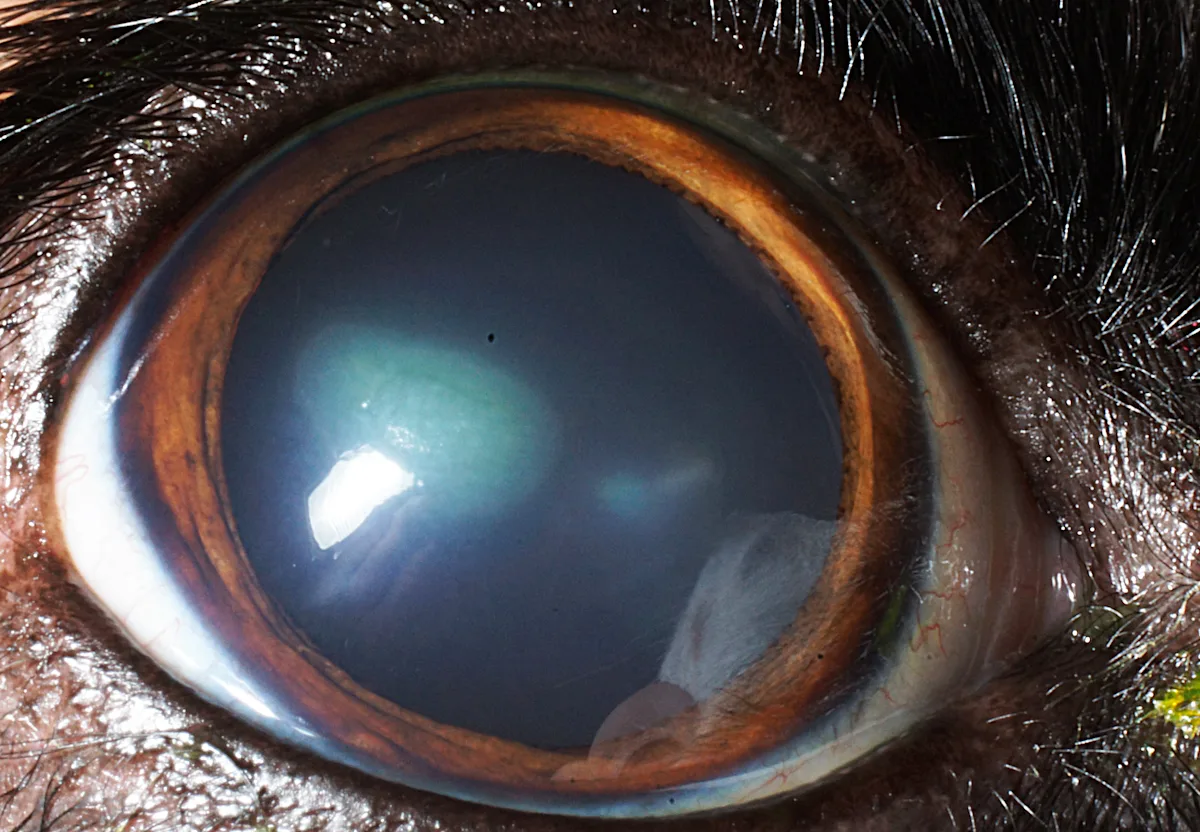
Typical staining pattern of an indolent corneal ulcer, with intense stain uptake at the center of the ulceration and a diffuse ring of less intense uptake (ie, halo sign)
Treatment
Therapy focuses on removing nonadherent epithelium from the superficial cornea to allow healthy epithelium to form and properly adhere to the basement membrane. Owners should be informed that multiple treatments may be required and recurrence is possible, as these patients are predisposed to forming subsequent indolent ulcers in the contralateral eye.
Patients may be initially managed with cotton-tipped applicator debridement alone, which has an ≈50% overall prognosis (anecdotal) for healing. Broad-spectrum topical antibiotic therapy should be administered every 6 hours to prevent infection and prepare for possible diamond burr debridement.
Healing should be assessed after 2 weeks; if the indolent ulcer has not healed, diamond burr debridement (75%-87% prognosis for healing after one treatment) or superficial keratotomy is recommended.4,5 The authors typically perform superficial grid keratotomy if diamond burr debridement is not effective, as using an additional method of debridement may aid in healing. Diamond burr debridement and superficial grid keratotomy are equally effective for management of indolent ulcers and have no difference in postprocedure complication rates.6
Diamond burr debridement can be performed in a general practice setting. Case selection is critical, as although diamond burr debridement can be used on superficial corneal ulcers not noted to be infected on examination, it cannot be used on stromal ulcers or ulcers with signs of infection or malacia because debridement can worsen infection. The authors recommend administering topical antibiotics (typically ofloxacin and oxytetracycline/polymyxin B) for 1 to 2 weeks prior to diamond burr debridement to aid in resolution of potential infections prior to the procedure. Although indolent ulcers are not typically infected, there is risk for keratomalacia if an infected ulcer is debrided. Sedation during the procedure may allow more thorough debridement and can help maintain patient comfort.
Posttreatment Care
Following debridement, patients should wear a rigid Elizabethan collar and continue to receive topical antibiotics every 6 hours until a 2-week recheck to help reduce the risk for infection of the compromised cornea and deepening the ulceration. Systemic NSAIDs and analgesics may also be administered for 2 weeks. Owners should be informed that although the eye may appear cloudy and red following debridement, patient comfort should increase by the recheck.
Step-by-Step: Diamond Burr Debridement for Indolent Corneal Ulcers
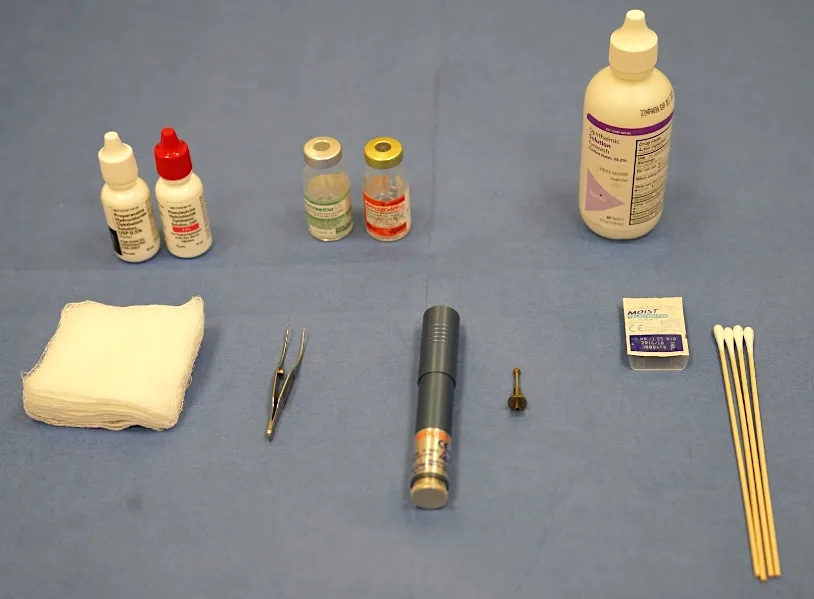
What You Will Need
Sedation (optional)
Eyelid speculum (optional)
Topical proparacaine
Topical ofloxacin
Sterile cotton-tipped applicators
Colibri forceps
Sterile eyewash
Diamond burr
Soft contact lens
Step 1: Administer Sedation (Optional)
Sedate the patient if indicated.
Author Insight
Sedation is not necessary but is recommended by the authors for more complete debridement and patient comfort. Depending on patient temperament, an eyelid speculum may be placed in an unsedated patient, and topical anesthetic may be sufficient.
Step 2: Administer a Topical Anesthetic
Administer one drop of proparacaine in the affected eye.
Step 3: Stabilize the Globe (Optional)
In sedated patients, grasp the conjunctiva just superior to the limbus with Colibri forceps to stabilize and allow manipulation of the globe.
Author Insight
Stabilization and ability to manipulate the globe helps ensure debridement of the whole cornea.
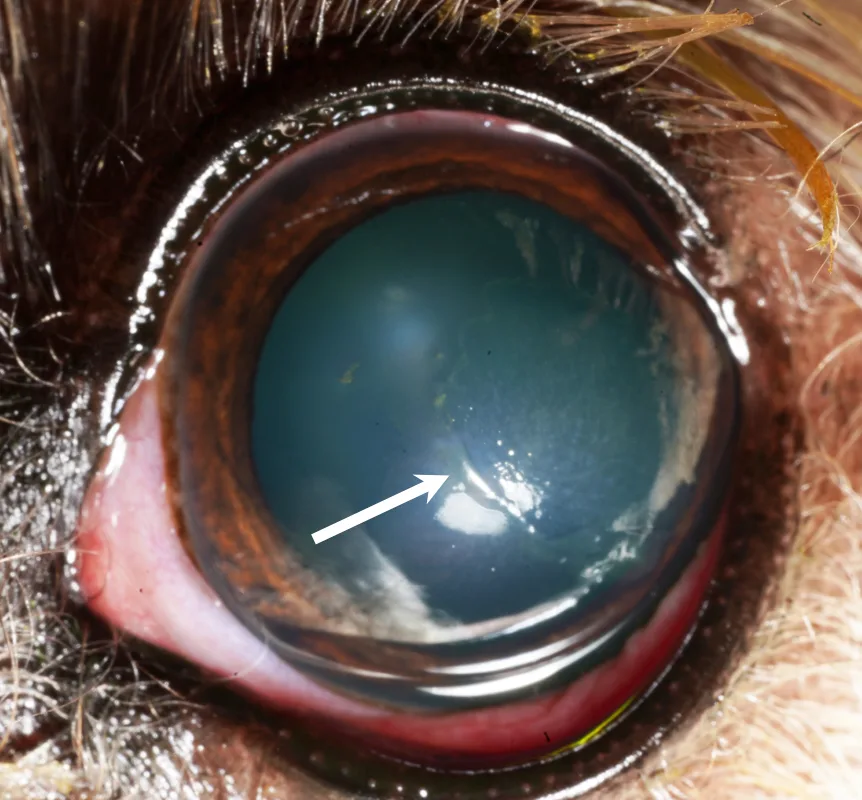
Step 4: Perform Cotton-Tipped Applicator Debridement
Use a sterile cotton-tipped applicator to debride excess loose epithelial tissue (arrow) until only adhered epithelium remains grossly.
Step 5: Perform Diamond Burr Debridement
Use a diamond burr to debride the cornea by making slow, circular passes with the burr perpendicular to the cornea until no loose epithelium is observed.

Author Insight
The diamond burr tip should be properly sterilized, and care should be taken to only contact the cornea with the tip. The tip should be discarded and replaced if haired skin or other tissue or items are touched.
The cornea will indent slightly when proper pressure is applied. The entire cornea should be debrided for a total of 45 seconds.7 Visualization of the entire ulcerated area is made possible by first performing a cotton tip applicator debridement. The cornea should have a characteristically dull appearance once it has been thoroughly debrided.
Eyewash irrigation of the cornea flushes debrided epithelium prior to placement of a contact lens.
Step 6: Place a Contact Lens
Place a soft contact lens onto the cornea.
Author Insight
A soft contact lens can increase the speed and likelihood of healing.8 The authors prefer 30-day balafilcon A lenses (diameter, 14 mm; base curve, 8.6 mm). The lens may fall out prior to recheck but does not need to be replaced. The owner should be instructed not to attempt replacement of the lens in the eye.
Step 7: Administer a Topical Antibiotic
Administer one drop of a broad-spectrum, bactericidal antibiotic in the affected eye.
Author Insight
If the patient is sedated, the antibiotic should be administered prior to reversal.
Listen to the Podcast
Want more tips from Dr. Haeussler? He joined the podcast to give more insight into these cases.