Conjunctivitis in Dogs: An Overview
Ron Ofri, DVM, PhD, DECVO, Hebrew University of Jerusalem

Conjunctival swelling and congestion with purulent discharge in a dog with conjunctivitis. Note that the palpebral, bulbar, and third eyelid conjunctiva, as well as the cornea, are inflamed.
Profile
Definition
Conjunctivitis is an inflammation of the conjunctiva, a tissue that lines the eyelids and covers the sclerae.
The conjunctiva is an exposed mucous membrane that reacts to antigenic stimulation caused by contact with noxious stimuli.
The superficial stroma of the conjunctiva is rich in lymphatic tissue, both diffuse and aggregated.
When aggregated tissue is stimulated, it forms lymphoid follicles, which produce effector cells. Conjunctival plasma cells produce specific immunoglobulins as part of the secretory component of the immune response.1,2
Causes
In dogs, primary conjunctival infections, particularly bacterial infections, are uncommon.
Most infections are caused by other diseases or disorders that trigger inflammation and may facilitate secondary, opportunistic bacterial infection.1,3,4
Keratoconjunctivitis sicca (KCS, or dry eye)
May be the most common cause of conjunctivitis in dogs (Figure 1)
Reported in one study as the cause of 1% of all conjunctivitis cases in North American Veterinary Medical Colleges.5,6
Allergies
Both eyes are affected and presentation may be seasonal.
Patients frequently present with concurrent atopic dermatitis.7,8
Local hypersensitivity reactions can be caused by insect stings, which result in acute but usually unilateral signs . They can also be associated with topical ophthalmologic medications.
Entropion
Inverted eyelashes and hair rub and irritate the conjunctival surface.
Ectropion
Exposes the conjunctival surface and may cause irritation.
Eyelash disorders (eg, distichiasis, trichiasis, ectopic cilia) and rubbing of the nasal folds against the conjunctiva
Overgrowth of normal flora, in particular, Staphylococcus spp or Streptococcus spp
Other infectious micro-organisms, including viruses (eg, distemper, canine herpesvirus 1), protozoa (Leishmania spp), fungi (Blastomyces dermatitidis), and parasites (eg, Thelazia spp, Onchocerca spp).9-12
History & Physical Examination
Affected dogs are typically presented with a history of red eye caused by conjunctival hyperemia and ocular discharge.
Clients may notice swelling of the conjunctiva (ie, chemosis), which, in some cases, may also cause third-eyelid elevation.
Other than the eye(s), the physical examination is unremarkable, unless conjunctivitis is a manifestation of a systemic disease (eg, distemper, leishmaniasis) or atopy.

Figure 2 Conjunctival hyperemia caused by engorgement of conjunctival blood vessels in a dog with KCS. Note the vascular invasion of the superficial cornea.
Clinical Signs
Clinical signs are mostly nonspecific1,3:
Hyperemia of conjunctival vessels (Figure 2)
Conjunctival edema (ie, chemosis), swelling, and thickening
Ocular discharge, which may be serous, mucoid, or purulent (Figure 3)
Hypertrophy of lymphoid follicles, particularly on the inner aspect of the third eyelid (Figure 4)
Conjunctival ulceration and subconjunctival hemorrhage
Concurrent corneal involvement (present in KCS; Figure 5)
Minimal ocular pain, but possible discomfort, expressed as mild blepharospasm
Diagnosis
Definitive Diagnosis
In dogs, conjunctivitis is rarely a primary disease.
Underlying cause should be established.13
Schirmer tear testing must be performed in every patient presented with conjunctivitis to diagnose or rule out KCS.
Possible qualitative tear disorders should not be ignored and should be ruled out by measuring tear film breakup time and carefully examining the meibomian glands for signs of meibomianitis.2,5,6
Eyelid conformation should be inspected carefully using magnification to rule out entropion or ectropion.
The ocular surface should be checked for irritating hair and eyelashes (Figure 6); the inner eyelid surface should be inspected for ectopic cilia, and the conjunctival fornices and inner aspect of the third eyelid should be examined for foreign bodies.
The patient should be evaluated for atopy, with particular attention paid to the eyelids, where dermal signs of atopy may be present.
A conjunctival provocation test using dust mite allergens may be considered.7,8
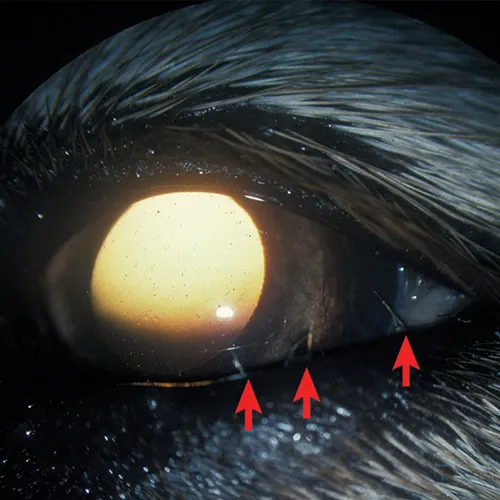
Figure 6 Distichiasis in a dog (red arrows). The eyelashes exiting through the orifices of the meibomian glands are a potential source of conjunctival irritation. Photo courtesy of Hebrew University of Jerusalem Seth Koch Slide Collection
Differential Diagnosis
A comprehensive systemic and ophthalmologic examination is indicated to rule out ocular manifestations of systemic diseases such as distemper or leishmaniasis.4,9,12
Other ophthalmologic diseases can result in conjunctival swelling but are not strictly defined as conjunctival inflammation. These conditions should be considered as differential diagnoses and include:
Orbital disease (eg, retrobulbar abscess or tumor, mucocele)
Conjunctival neoplasia13 (Figure 7)
Scleral inflammation (eg, scleritis, necrotizing or non-necrotizing granulomatous scleritis)
Prolapsed orbital fat
Onchocerca spp granulomas
Conjunctival hyperemia is a clinical sign of anterior uveitis and glaucoma.
Appropriate testing for these conditions should be performed.
Laboratory Findings
Cytologic findings are typically not helpful in reaching a diagnosis.
Neutrophils are usually associated with acute (bacterial or viral) conjunctivitis, whereas plasma cells and lymphocytes characterize an immune-mediated response and more chronic cases.
Specific causes of canine conjunctivitis are rarely identified through cytology.13-15
Occasionally, cytology may aid in the diagnosis of an allergic response (indicated by the presence of eosinophils) or an infectious agent such as Leishmania spp.
Other histopathologic findings, including changes in goblet cell density, papillary hypertrophy, and formation of inflammatory membranes or pseudomembranes, can also indicate chronic conjunctivitis but do not help in establishing its cause. 1,9,10,13,14
Conjunctival biopsy may establish lymphoma, rather than conjunctivitis, as the cause of conjunctival swelling.
Bacterial culture and susceptibility testing are not indicated in the initial diagnostic plan, as ocular discharge samples usually will yield overgrowth of gram-positive organisms that are part of the normal conjunctival microbiota.1,3,13,14
Such testing should be considered only in later stages, if no primary cause is identified and the infection does not respond to treatment.3,8,16
Treatment
In most cases, the key to successful treatment is correctly diagnosing and addressing the primary cause.
Tear production should be increased and stabilized in KCS patients via administration of lacrimomimetic and lacrimogenic agents.17
Conjunctivitis caused by eyelid or eyelash disorders usually is resolved surgically.
Allergic conjunctivitis is treated through avoidance of the inciting allergen, hyposensitization, and topical glucocorticoids and/or antihistamines.7,8
Once the primary disease has been successfully treated, any residual conjunctival inflammation or infection usually responds to topical glucocorticoids and topical broad-spectrum antibiotics.1
Follow-up
Patient Monitoring
Persistent hypertrophy of the conjunctival lymphatic follicles is common and can cause local irritation and discomfort, even after conjunctivitis has been treated successfully.1,3,13,14
Irritation may resolve with saline irrigation and supportive treatment with topical dexamethasone.
Alternatively, the follicles may be debrided using dry gauze or the blunt end of a scalpel blade.
If the patient does not respond to treatment or conjunctivitis recurs, the initial diagnosis, rather than the treatment choice, should be re-evaluated.
Complications
Complications can occur if the primary cause of conjunctivitis has not been identified.
For example, distemper and leishmaniasis manifest as systemic diseases; eyelid and eyelash disorders and dry eye may also affect the cornea and cause keratitis or corneal ulceration.
Because of the proximity of the conjunctiva to the cornea, infectious conjunctivitis may spread to the cornea, resulting in keratoconjunctivitis and possible corneal ulceration.
Prognosis
If the primary cause of conjunctivitis has been identified and treated successfully, most cases will resolve with topical glucocorticoid and/or topical broad-spectrum antibiotic treatment.
If the primary cause of conjunctivitis has not been identified and treated, use of topical glucocorticoids and/or topical broad-spectrum antibiotics will treat signs only, and conjunctivitis most likely will recur once treatment is discontinued.
Editor's note: This article was originally published in April 2017 as "Conjunctivitis in Dogs"