Chronic Regurgitation in a Puppy
Ryan Taggart, DVM, MS, DACVS-SA, Adelaide Veterinary Specialist & Referral Centre, Adelaide, Australia
Daniel F. Hogan, DVM, DACVIM (Cardiology), Purdue University

A 5-month-old, 9.8-kg intact male Siberian husky was presented for chronic regurgitation after meals.
History
When the dog was approximately 6 weeks of age, he started regurgitating undigested food 10 minutes to 2 hours following meals. The episodes were occasionally accompanied by coughing and abdominal effort. After the owner started feeding smaller meals more often, the episodes became less frequent. Despite having a voracious appetite, the dog was thin compared with its littermates. No medication was given to relieve the signs.
Examination
The dog was alert, responsive, and appeared to be well hydrated. All examination parameters appeared to be within normal limits and the body condition score was 4/9.
Which of the following should be included on the initial differential diagnosis list for Charlie’s regurgitation?
Being an excellent veterinary diagnostician depends on a solid foundation in the basics. Explore more differential list challenges in our General Practice Skills series here.
Diagnostics
Packed cell volume, total protein, and whole blood glucose results were within normal limits. Right and left lateral and VD thoracic radiographs were taken (Figure 1).

VD view of thorax: Note leftward deviation of the trachea just cranial to the cardiac silhouette.
Ask Yourself
What are the diagnostic differentials for this presentation?
What additional diagnostics could be performed, and what relevant information would they provide?
What is the prognosis for patients with this condition?
Diagnosis
Persistent right aortic arch (vascular ring anomaly)
Episodes of regurgitation shortly after weaning are consistent with esophageal obstruction seen with vascular ring anomaly. Persistent right aortic arch (PRAA) with a left ligamentum arteriosum is the most common vascular ring anomaly in dogs, representing 95% of cases. German shepherds and Irish setters are overrepresented.1 Affected patients may be predisposed to aspiration pneumonia from chronic regurgitation or esophageal dysmotility.
A barium esophagram identified esophageal narrowing at the base of the heart with dilation of the esophagus orad to the narrowing (Figure 2). Esophageal function distal to the constriction appeared normal.
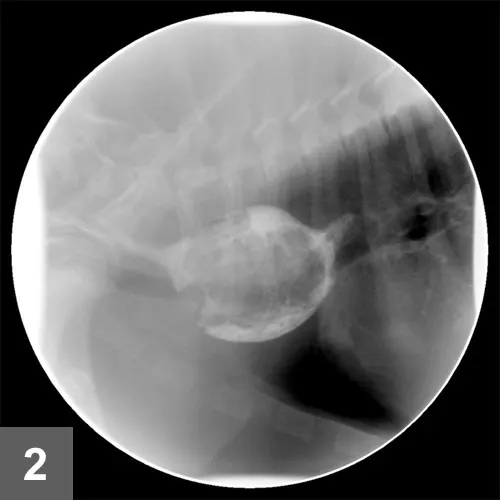
Lateral view of contrast esophagram: Note the esophageal dilation cranial to the cardiac silhouette.
Treatment
A left 4th intercostal thoracotomy was performed to isolate and transect the left ligamentum arteriosum (Figures 3 & 4).
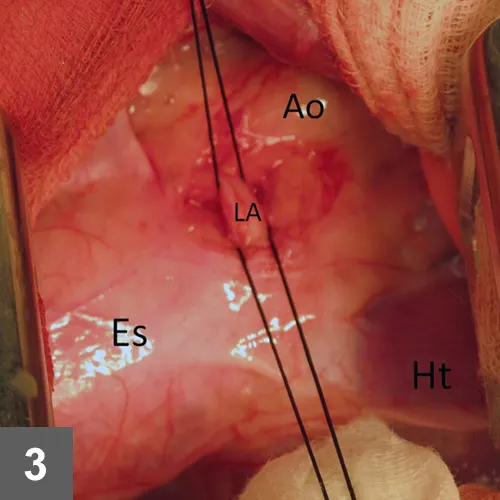
Intraoperative view: The left ligamentum arteriosum (LA) is isolated with 2-0 silk. The dilated esophagus (Es) cranial to the heart (Ht) is clearly visible; Ao = aorta.
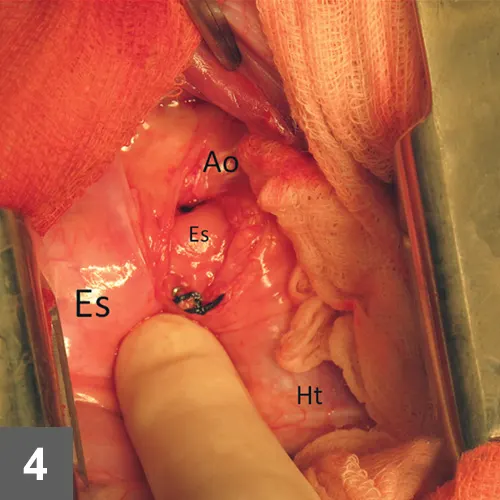
Intraoperative view: The left ligamentum arteriosum has been divided, exposing the entrapped esophagus (Es); Ht = heart, Ao = aorta
To identify any periesophageal fibrous bands, a Foley catheter was advanced past the area of the stricture; the bulb was inflated and drawn orad to dilate the esophagus at the level of the stricture. Remaining fibrous bands were isolated and released. Plication of the dilated esophagus was not performed, as it is associated with increased risk for complications and contributes little to improved function.1 The patient was discharged 2 days after surgery.
Outcome
Two weeks after surgery, the patient was bright and alert. His appetite remained voracious and the owner continued feeding small, frequent meals with no episodes of regurgitation. Telephone follow-up 1 month after surgery confirmed that the dog was gaining weight and had experienced no episodes of regurgitation. The owner was advised to slowly introduce larger, less frequent meals.
A barium esophagram identified esophageal narrowing at the base of the heart with dilation of the esophagus orad to the narrowing (Figure 2). Esophageal function distal to the constriction appeared normal.
Did You Answer?
What are the diagnostic differentials for this presentation?
Diagnostic differentials include generalized megaesophagus, esophageal obstruction caused by foreign body, esophageal stricture, focal esophageal weakness, intra- or extraluminal mass, or hiatal hernia.
What additional diagnostics could be performed, and what relevant information would they provide?
Recommended diagnostics for dogs that begin regurgitating shortly after weaning:
Plain thoracic radiography is typically sufficient to diagnose vascular ring anomaly. Focal leftward deviation of the trachea near the cranial border of the heart in DV or VD radiographs is a reliable sign of PRAA.2
Complete thoracic radiographic series can identify concurrent pneumonia.
Contrast esophagography using barium can document esophageal stricture at the level of the heart base.
Fluoroscopy is beneficial in evaluating esophageal motility, especially distal to the constricted area, which may affect prognosis.
Endoscopic evaluation can exclude foreign body, mass, stricture, or focal weakness as causes of chronic regurgitation.
CT angiography provides 3-dimensional appreciation of the vessel architecture and may help identify coexisting anomalies, such as PRAA with persistent left ligamentum arteriosum and left subclavian artery. The coexistence of a retroesophageal left subclavian artery is present in approximately one-third of PRAA cases and can often go unrecognized.2
What is the prognosis for patients with this condition?
In patients with PRAA, prognosis after surgical correction has improved significantly over the past 40 to 50 years (see Consider This). Continued regurgitation is the most common problem encountered after surgery, leading to increased risk for aspiration pneumonia. The presence and severity of aspiration pneumonia before surgery can adversely affect the prognosis. In addition, the extent of esophageal constriction and dilation, degree of esophageal dysfunction, medical management before and after surgery, and severity of debilitation before surgery can all influence the prognosis.5 A gastrostomy tube may be considered for both pre- and postoperative nutritional support.6
Consider This
A reported series of 232 dogs with PRAA found a postoperative survival rate of 80% at 3 weeks but an excellent postsurgical outcome in only 9% of cases.3 A subsequent case series found a 94% postoperative survival rate at 2 weeks and an excellent postsurgical outcome in 92% of cases.4 The authors of the latter study suggest that paying increased attention to the release of periesophageal fibrous bands and performing esophageal bougienage may contribute to improved outcome, along with earlier disease recognition. Despite current recommendations to perform surgery as early as possible, there is no clear evidence that doing so when dogs are young carries a better long-term prognosis than delaying the procedure until dogs are older.1