In the Literature
Maggiar A, Andréjak-Bénit J, Miclard J, Sarran D, Billet J-P. Intestinal full-thickness needle-core biopsy via laparotomy is safe, rapid, and effective and less invasive than standard incisional biopsy in dogs and cats. J Am Vet Med Assoc. 2023;262(4):1-7. doi:10.2460/javma.23.09.0521
The Research …
Intestinal biopsy is used to determine the underlying cause of chronic diffuse intestinal disease in cats and dogs. For most diffuse intestinal disease, full-thickness biopsy samples from the duodenum, jejunum, and ileum are recommended for histopathologic analysis with or without immunohistochemistry. Partial-thickness endoscopic biopsy samples can be helpful but may not be adequate to distinguish between small intestinal disorders (eg, intestinal lymphoma vs inflammatory bowel disease). The ideal sampling technique should be minimally invasive and provide an adequate full-thickness tissue sample for analysis with minimal risk for postoperative dehiscence.
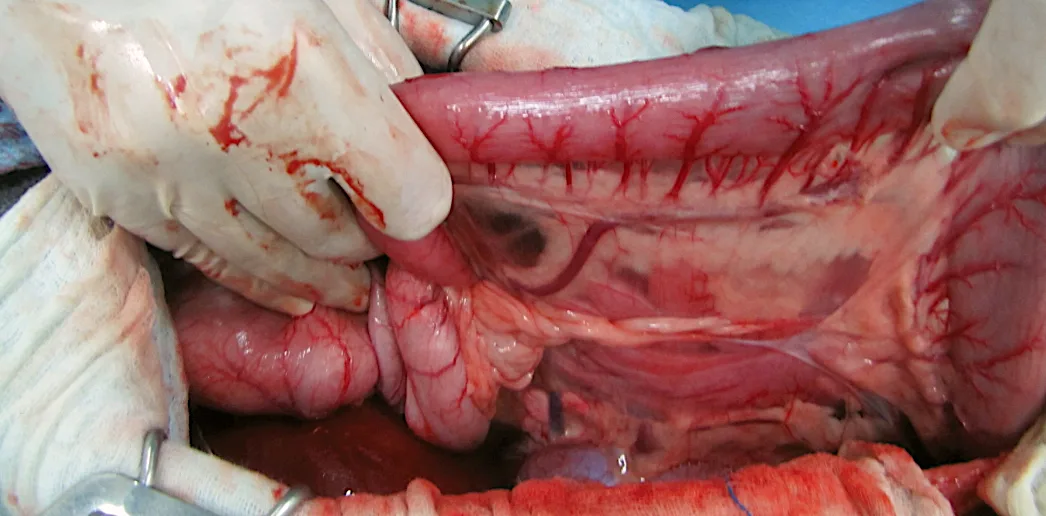
This prospective study evaluated the safety and diagnostic efficacy of full-thickness intestinal sampling during laparotomy using a needle-core biopsy technique, comparing results with traditional incisional biopsy. Cats (n = 17) and dogs (n = 3) with chronic diffuse intestinal disease had one traditional incisional biopsy sample collected from each area of the small intestine (ie, duodenum, jejunum, ileum) and 2 needle-core biopsy samples collected 1 centimeter cranial and caudal to each incisional biopsy site. Incisional biopsy sites were closed with a simple continuous suture pattern, and needle-core biopsy sites were closed with a single interrupted suture. Key clinical data from each patient included histopathologic and immunohistochemical findings, biopsy collection times, and complications over a 2-week follow-up period.
Needle-core biopsies were completed safely with no associated major complications. One cat with pre-existing bile peritonitis experienced postoperative dehiscence at the incisional jejunal biopsy site and died; adjacent needle-core biopsy sites remained closed. Both types of biopsies were performed in a clinically reasonable amount of time, but the needle-core technique was significantly faster (mean, 262 seconds vs 599 seconds for incisional biopsy). The authors found 100% agreement between biopsy techniques when differentiating intestinal lymphoma and inflammatory bowel disease via histopathology and immunohistochemistry. In cases of inflammatory bowel disease, there was high agreement (90%-100%) between biopsy techniques for histologic categorization as lymphoplasmacytic, eosinophilic, or neutrophilic.
… The Takeaways
Key pearls to put into practice:
Needle-core biopsy can be quick and safe when performed via abdominal laparotomy with single-suture biopsy site closure in patients with diffuse small intestinal disease.
Although biopsies were performed with an open surgical approach in this study to establish safety and diagnostic efficacy, the needle-core technique may help simplify laparoscopic intestinal sample collection.
Authors of this study recommend inserting the needle-core biopsy device at a 45-degree angle in an antimesenteric location to reduce the risk for accidental puncture of the mesentery. The oblique defect made by an angled needle may also help reduce the risk for site leakage. Maintaining close contact between the inner stylet of the device and intestinal wall during device deployment is also recommended to reduce the risk for sample loss into the lumen during retrieval.
You are reading 2-Minute Takeaways, a research summary resource presented by Clinician’s Brief. Clinician’s Brief does not conduct primary research.