Anesthetic Monitoring: Interpreting the Readings
Cheryl Irzyk Kata, RVT, VTS (Anesthesia), CVPP, North Carolina State University Veterinary Teaching Hospital
Confident in your anesthetic monitoring skills? Check out Quiz: Anesthesia Monitoring here!
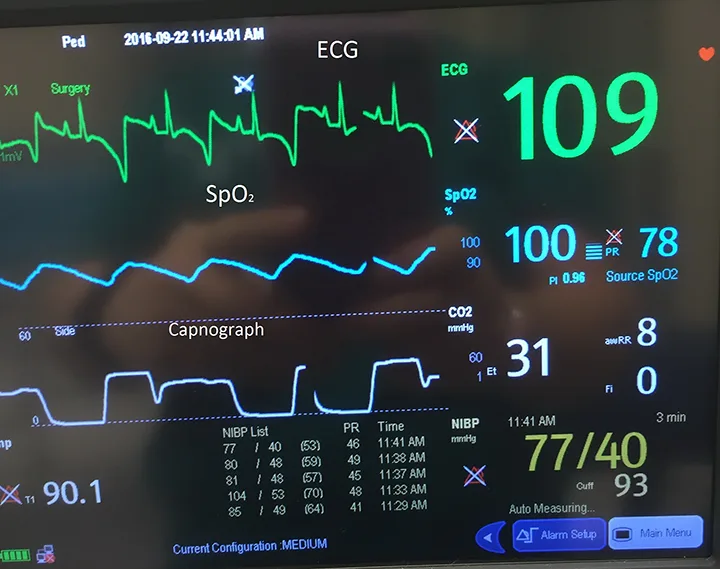
Monitors, from the simple pulse oximeter to the multiparameter monitor that measures arterial blood pressure and capnography, have changed the world of veterinary medicine. They have enabled veterinary teams to handle delicate cases with excellent results. In the 1970s and 1980s, veterinary medicine relied on visual, tactile, and auditory skills for patient monitoring. Although these skills are still important, the monitoring observations may not reveal the complete story of patient status and therefore should not be relied on solely when making decisions about the patient.
However, a monitor cannot save a patient’s life unless the team member monitoring the patient understands the readings and can determine when the monitor is wrong. Any values differing from normal parameters should be investigated to determine whether they are life-threatening or merely glitches in the equipment or setup. (See Table 1.)
Table 1: Normal Parameters
For a normal, healthy patient, the monitor should display readings within the following parameters.
aMay vary depending on the medications used or the patient’s health status
bVaries depending on the patient’s size
Pulse Oximetry
A noninvasive pulse oximeter can be used on an awake or anesthetized patient. The instrument measures the amount of oxygen saturated in hemoglobin over a pulsating vascular bed (eg, tongue, hairless skin fold, hairless ear area, vulva, prepuce, between toes).
How Pulse Oximetry Works
Common pulse oximetry probes include the regular pressure clip, which can be placed on a pulsating vascular bed; the reflectance probe, which can be taped under a shaved spot on the tail or to a hairless spot on the skin; and the rectal probe, which can be inserted into the rectum. To obtain the patient’s SpO2 level, these instruments send red and infrared light though the pulsatile arterial bed.3 As the light passes through the arterial bed, it determines if the hemoglobin is saturated with oxygen. (See Figure 1.) The SpO2 level should be kept above 95%, which means the patient’s arterial oxygen blood level is 80 mm Hg.1 If the patient is breathing room-temperature air at sea level, this measurement is within normal limits.
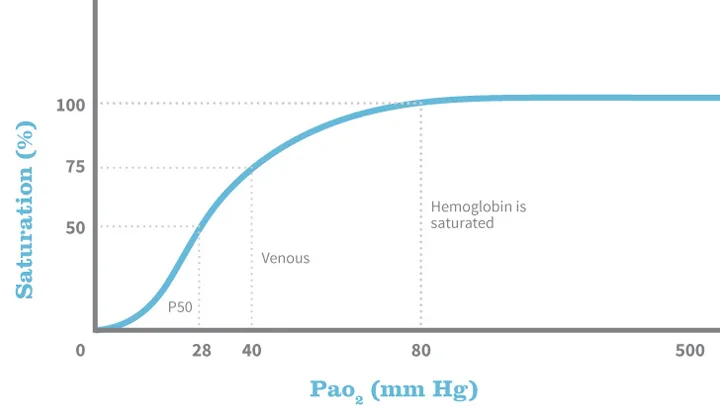
Oxygenated hemoglobin (HbO2) dissociation curve
Reasons for False Readings
Although the SpO2 reading is a useful parameter to follow, it does have some limitations. Depending on the combination of drugs given, if the patient develops peripheral vasoconstriction, SpO2 readings may not render accurate results. Some drugs, including α-2 adrenergic agonists (eg, dexmedetomidine, xylazine), can initially cause peripheral vasoconstriction and may limit the accuracy of information derived from the pulse oximeter.3,4
Movement, whether actual movement in the case of an awake patient, movement caused by the surgeon, transport to and from the procedure, or shivering in a patient recovering from anesthesia, may affect the pulse oximetry reading.
Other factors that may impact the SpO2 reading include surgery lights interfering with the sensor’s light waves, hypothermia without shivering, hypotension, carbon monoxide poisoning, methemoglobinemia, and occlusion of the pulsatile arterial bed. (See Figure 2.)
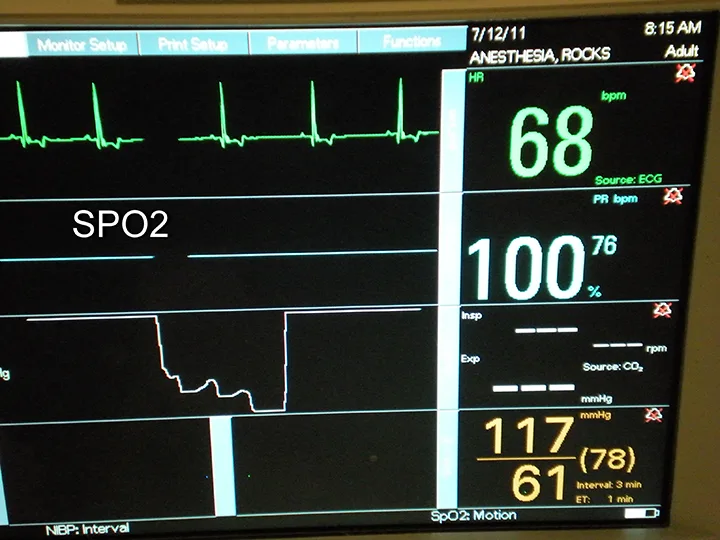
No wave on SpO2
If no wave is associated with the number on the pulse oximeter, the reading displayed could be false. In that case, reposition the probe and wait for a wave to confirm the reading.
Capnography
Capnography, perhaps the most underused monitoring device in veterinary medicine, is a noninvasive, real-time monitor of the CO2 level in the patient’s respiratory cycle.3 Capnograph units are typically easy to use and require no previous training.
Capnograph units are also highly accurate, especially those that produce graphs displaying the patient’s ventilatory status. However, team members who do not understand how the equipment works can arrive at false conclusions.
The most important monitoring step is to pause and ensure the patient is breathing because the capnometer works on a breath-by-breath basis. If the patient has been disconnected from the circuit, is not breathing, or has died, the capnograph will be zero. If the capnograph is zero, manually give the patient a breath, ensure the capnograph registers this breath, and visually assess the patient’s chest to ensure movement. If the chest rises and the mucous membranes are pink (ie, SpO2 >95%), look for other problems (eg, occlusion of the capnometer line, patient detachment from the breathing circuit, patient’s anesthetic depth is too deep to ventilate properly). (See Figure 3.)
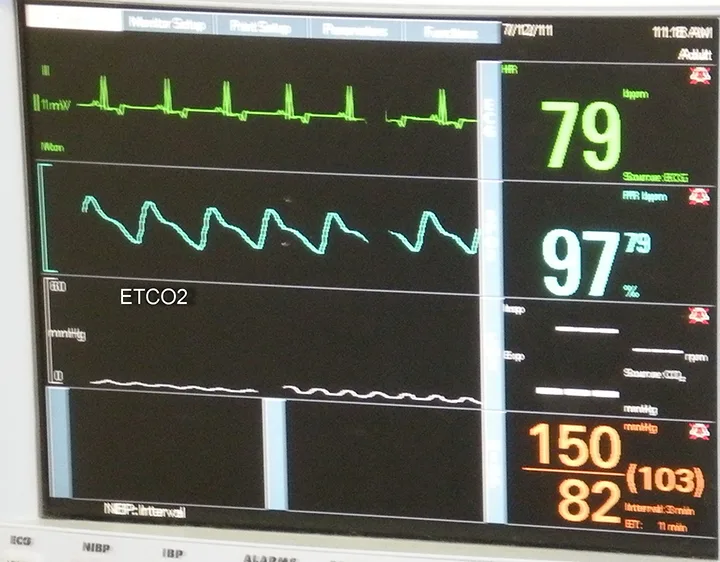
No capnography wave
The capnograph can also indicate inspired CO2, which should be zero. If the capnograph wave does not go to zero, a one-way valve on the anesthesia machine may not be properly seated, the soda lime’s crystals are exhausted, or the fresh gas flow rates are inadequate.5 The capnograph can also be used to confirm proper endotracheal tube placement and to evaluate efficiency of CPR compressions. (See Figure 4.)
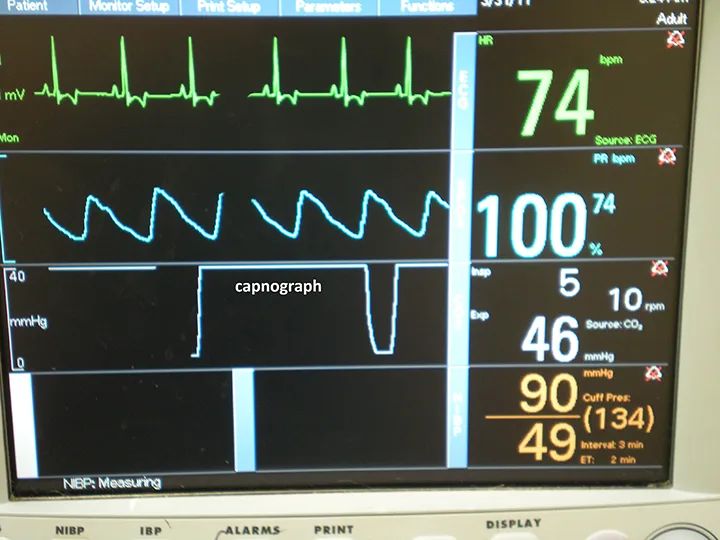
Capnograph wave does not go to zero
Blood Pressure
The gold standard for measuring blood pressure is an indwelling arterial catheter connected to a pressure transducer. The blood pressure measurements obtained from this device are accurate and reproducible. However, this invasive procedure has its drawbacks (ie, special training and equipment is required, the patient can rapidly lose a large quantity of blood if the catheter end slips off). For most healthy, non-life-threatening surgical procedures, the indirect, noninvasive, oscillometric blood pressure measurement is used. This monitor provides less accurate readings than the indwelling arterial catheter, however, and should be viewed as an overall trend rather than exact numbers.3
An oscillometric blood pressure cuff can give varied results depending on the cuff size. Cuffs too wide for the site (eg, limb, tail) will underestimate the blood pressure. The reverse is true for a cuff that is too narrow. A properly fit cuff should be 40% of the circumference of the limb or tail.3 (See Figure 5.)

Blood pressure cuff is too large for the patient
Considering that the oscillometric blood pressure cuff readings tend to be a trend and not an exact number, mean arterial pressure (MAP) should be kept above 60 mm Hg. If the MAP is trending downward during surgery, interventions should begin early to avoid poor perfusion to organs and prolonged hypotension.
Electrocardiography
The ECG measures the electrical current generated by the heart. When using a 3-lead ECG, only heart rate and rhythm should be considered when making determinations about the cardiovascular system.3,6 The ECG also will not evaluate the efficiency of the heart to pump blood; if used as a sole monitor, it can mislead the anesthetist by producing a rhythm called a pulseless electrical activity (PEA). PEA occurs when the ECG waveform displays on the monitor as a normal wave, but the heart has stopped beating. A multiparameter monitor is therefore critical so all parameters can be assessed simultaneously. If a PEA is noted, then ETCO2 and SpO2 will be decreased or nonexistent.
The ECG may also double count the heart rate. This occurs when large T waves are counted as R waves and can be noted when the ECG heart rate is 1.5 to 2 times as much as the SpO2. To determine the correct heart rate, manual manipulation of a pulse should be performed. (See Figure 6.)
Double counting on the ECG
Conclusion
Monitors are a useful addition to veterinary medicine, but they do not replace careful monitoring by the veterinary nurse. Visual, tactile, and auditory skills are still critical in the monitoring process. Remember, the anesthetist is the smartest monitor in the room.
This article originally appeared in the May 2017 web issue of Veterinary Team Brief.