Acute Moist Dermatitis
Erin E. Aufox, DVM, University of Tennessee
Linda A. Frank, MS, DVM, DACVD, University of Tennessee
Laura F. Grieco, DVM, MLAS, University of Tennessee

AMD on the caudal dorsum of a German shepherd dog; matted hair makes visualization of the lesion difficult.
Acute moist dermatitis (AMD), commonly referred to as hot spots, typically results from self-inflicted trauma in response to painful or pruritic stimuli.<sup1- 4sup> Although AMD typically only involves surface bacterial colonization (ie, overgrowth)—not true infection—lesions may progress quickly and result in folliculitis and, sometimes, furunculosis, especially without treatment.4,5
Fleabite hypersensitivity is a primary inciting factor of AMD; lesions typically develop shortly after flea exposure.2,3 Other inciting factors can include ectoparasites, otitis externa, foreign bodies, irritating substances, and skin diseases that result from allergic dermatitis.<sup1- 4sup> In dogs, AMD can occur in both sexes and all ages and breeds, with male dogs <4 years and certain breeds (eg, golden retrievers, German shepherd dogs, collies, Saint Bernards) overrepresented.1,4,5 Dogs with heavy and dense undercoats are more susceptible to developing hot spots as a result of increased environmental temperatures and slow drying of the coat due to lack of proper ventilation, which can result in conditions that are favorable for bacterial overgrowth.1
History & Clinical Signs
Patients with AMD are typically presented subsequent to sudden onset of intense pruritus localized to one area of the body.1-3 Owners often report that no lesions existed hours prior to presentation. Patients with AMD may not receive regular or adequate flea preventive, and flea hypersensitivity is common. Typical lesion locations include the caudal dorsum and other areas the patient can reach with its mouth (Figure 1). In addition, lesions may be present on the lateral face under the pinnae and rostral to the neck.1 Lesions may be flat, moist, and exudative, with erosion and/or ulceration in the center.1,4,5 The patient’s hair is often matted,1 which can inhibit accurate visual examination of the lesion until after the area is clipped. Bacteria typically colonize the surface of AMD lesions, and superficial or deep pyoderma may be present in some cases.5 Satellite lesions adjacent to the clipped primary lesion may be suggestive of folliculitis or furunculosis (Figures 2 and 3).1,5 Lesions on the lateral face (made by scratching instead of licking or chewing) appear clinically similar to classic superficial hot spots but have often developed into deep pyodermas by the time they are evaluated by a clinician.1,5 Recognizing when AMD lesions are complicated by folliculitis or furunculosis can lead the clinician to alter recommended therapy (eg, length and frequency of topical treatment, oral antibiotic therapy, bacterial culture and susceptibility testing) and thus improve clinical outcomes.

AMD secondary to otitis externa at the base of the ear. The lesion has been clipped, and satellite lesions (arrow) are evident.

Clipped lesion of the dog in Figure 1. Satellite lesions (arrow) indicate folliculitis or furunculosis, not surface colonization (ie, overgrowth).
Diagnosis
Diagnosis of AMD should be based on patient history, clinical signs, and elimination of other differential diagnoses (eg, folliculitis and furunculosis, acral lick dermatitis [Figure 4], dermatophytosis, localized demodicosis, neoplasia, calcinosis cutis).6 Impression cytology of AMD lesions, obtained by squeezing the lesion and applying a glass slide to the surface, can reveal numerous neutrophils, extracellular cocci, and, occasionally, bacilli. Intracellular bacteria may also be present in cases of folliculitis or furunculosis. If indicated, a culture can be obtained from these lesions by first cleaning the surface with chlorhexidine solution and rinsing with sterile water to remove the surface bacteria and oral flora, then rubbing a sterile culturette on the surface of the lesion after squeezing. Similar to what is found in cases of superficial pyoderma, Staphylococcus pseudintermedius is typically isolated from AMD lesions.5 Histopathology is not commonly performed when AMD is suspected but can be used to rule out differential diagnoses for persistent lesions and confirm cases of folliculitis or furunculosis. In a study of 44 dogs with AMD, 54% of dogs had epithelial necrosis or ulceration with superficial neutrophilic (± eosinophilic) dermatitis and edema and 45% had evidence of folliculitis and/or furunculosis regardless of location.1 An earlier histopathologic study revealed similar results.5
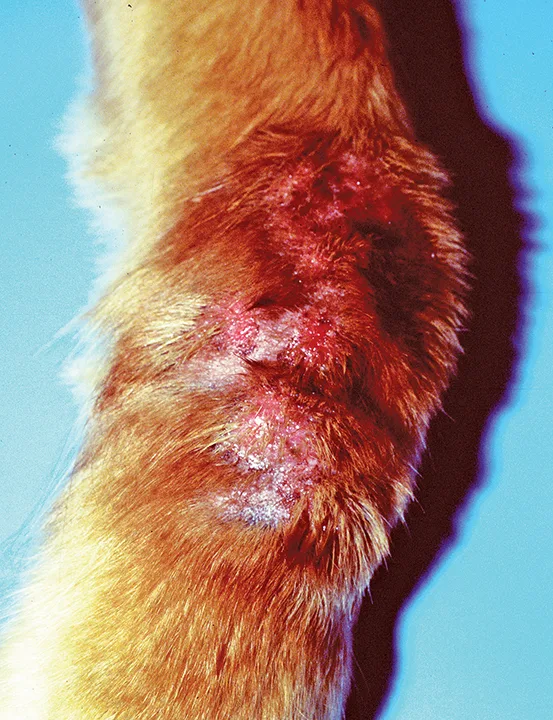
Acral lick dermatitis of the thoracic limb. Fibrosis indicates this is not an acute lesion and should not be confused with AMD.
Treatment & Management
Treatment of AMD should begin with clipping the hair of the affected area, taking care to prevent further trauma to the skin.2-4 Clipping should be performed beyond the visibly affected margin, as lesions often extend into the haired skin and can be difficult to visualize. Once the area is clipped, the area around the primary lesion should be examined to locate satellite lesions. Folliculitis or furunculosis is likely when satellite lesions are present and may necessitate the need for systemic antibiotics.1,3 The affected area should then be cleaned with a topical biocidal solution (eg, 2% chlorhexidine solution).3,7 If lesions are infected based on cytologic findings, topical treatment (eg, 2% chlorhexidine solution, antimicrobial spray or mousse containing chlorhexidine or ethyl lactate) should be used twice daily until lesions resolve. Medicated shampoos can be used alone if clipping the hair is not possible, although treatment failure may result. Systemic antibiotics are indicated if topical therapy does not resolve the infection or if areas are difficult to treat topically (eg, when infection extends into skin covered in dense hair).3,8 As with generalized pyoderma, empiric therapy should be based on typical susceptibility patterns of S pseudintermedius6; amoxicillin or penicillins should be avoided due to the prevalence of β-lactamase–mediated acquired resistance to these antibiotics found in S pseudintermedius isolates.1,9 Cephalexin (22-30 mg/kg q12h) is favored instead. Cefpodoxime (5-10 mg/kg q24h), a third-generation cephalosporin, has a similar spectrum of activity against Staphylococcus spp as compared with cephalexin and is often used in smaller animals to enable appropriate administration. Clindamycin can also be used empirically; however, resistance to this antimicrobial may occur.8 Antibiotics should be prescribed for an appropriate length of time, just as with other presentations of folliculitis or furunculosis. The standard course of therapy is typically 3 to 4 weeks (continued 1 week past clinical resolution) for superficial infections and 6 to 8 weeks (continued 2 weeks past clinical resolution) for deeper lesions.8
Antipruritic medications and, for some patients, an Elizabethan collar are also indicated, as self-trauma is key in lesion creation and perpetuation. A short course (ie, 3 days to 2 weeks) of anti-inflammatory prednisone or prednisolone (0.5-1.1 mg/kg) is recommended because fleabite hypersensitivity is often present and typically steroid responsive. Antimicrobial medications should be continued beyond discontinuation of steroids, as steroids can decrease lesion inflammation and obfuscate whether infection is truly resolved.6,10 Continuing antimicrobial medication until the skin has completely normalized (for topical medications) or is past clinical resolution (for systemic antibiotics) should help prevent relapse and recurrence. Other antipruritic options include labeled doses of oclacitinib and injectable caninized IL-31 monoclonal antibody. It is the authors’ opinion that potent topical steroids (eg, betamethasone, isoflupredone, triamcinolone) with or without topical antibiotics (eg, gentamicin, neomycin) should be avoided when treating AMD. Topical steroids may enhance bacterial growth or decrease localized antimicrobial defenses; often contain alcohol when formulated as a solution, which stings when applied to ulcerative lesions; and can counteract the patient’s local healing and immune responses, which can delay healing and perpetuate and exacerbate localized alopecia.2,11 In addition, the potential adverse effects of topical steroids—including iatrogenic Cushing’s disease, skin fragility, focal or generalized alopecia, and calcinosis cutis12—may not be fully understood by pet owners, which can lead to frequent and indiscriminate use of these products, further complicate cases, and prolong patient morbidity.
Prevention of AMD recurrence requires identifying and addressing the underlying cause. Because fleabite hypersensitivity is commonly associated with AMD, clinicians should ensure all pets in the household are receiving a consistent, high-quality flea preventive. Patients with AMD on the lateral face should be assessed for otitis externa.2 Once a patient is diagnosed with AMD, a recheck examination should be performed 3 to 4 weeks after the initial visit, thus helping to ensure clinical resolution and determination of when antimicrobial therapy can be discontinued.
Conclusion
AMD, like most dermatologic conditions, is not imminently life-threatening but can result in significant patient discomfort. Prevention of this condition can improve patient quality of life. Regular administration of high-quality ectoparasite control and vigilant monitoring and investigation of pruritus can be key to prevention of AMD.