Cryptorchid Neuter
Daniel D. Smeak, DVM, DACVS, Colorado State University
In dogs and cats, cryptorchidism is a condition in which one or both testicles have failed to descend into the scrotum generally by 2 to 4 months of age.1 In dogs, incidence ranges from 1% to 15% depending on the distribution of breeds in the study region.1 Most patients with cryptorchidism do not show signs of illness unless testicular neoplasia or torsion have developed.
Cryptorchid testicles can be situated in the original location of fetal testicular development, around the caudal pole of the kidney, along the path of testicular descent, in the inguinal ring, or in the subcutaneous tissue between the ring and base of the scrotum.2
In dogs, ≈50% of cryptorchid testicles are intra-abdominal; in cats, most ectopic testicles (ie, testicles located anywhere other than in the scrotum) are found in the inguinal region.3 Because cryptorchid testicles may appear small or atrophied and may not be readily palpable (particularly in cats), determining ectopic location and planning surgery can be challenging.
History & Clinical Signs
A thorough patient history should be obtained and a complete physical examination performed. Further diagnostic tests are warranted to determine neuter status or presence of retained testicular tissue in dogs with an unknown neuter history and no palpable testicles on examination. This is particularly important if there are signs of feminization or evidence of a concurrent condition (eg, prostatic disease, perineal hernia, perianal adenoma) overrepresented in intact dogs. Congenital absence of one (ie, monorchism) or both (ie, anorchism) testicles has been reported but is rare in small animals.4,5
Cats lose testosterone-dependent penile spines within 13 to 24 weeks of being neutered, so cats with penile spines and/or cats that demonstrate urine spraying or produce odiferous urine and have no palpable testicle(s) should be further evaluated using hormonal testing.6
Diagnosing Cryptorchid Testicles
Retained Testicles
If a retained testicle is suspected, hormone tests should be pursued to evaluate potential retained functional testicular tissue. Both human chorionic gonadotropin (HCG) stimulation and anti-Müllerian hormone biomarker tests can determine if a dog or cat has retained functional testicular tissue.
The anti-Müllerian hormone concentration in neutered or anorchid dogs is expected to be low (0.08-0.12 ng/mL) as compared with the concentration cutoff value (>5.5 ng/mL) in intact or cryptorchid dogs.7,8 For the HCG stimulation test, a baseline serum sample for testosterone levels should be collected, HCG (50 IU/kg) should be administered IM, and a second sample should be collected 2 hours later. A significant rise (>100%) in testosterone levels in the postinjection sample can indicate functional testicular tissue.9
Ectopic Testicles
If only a single testicle is found in the scrotum, the testicle should be pushed both dorsally and cranially toward the prescrotal region. The testicle will then move to one side of the midline, and the side it moves toward should be noted. The ectopic testicle will be on the contralateral side. Ectopic testicles in the prescrotal region, unless severely atrophied, can be readily identified and are rarely confused with other structures. Those located in or just external to the inguinal rings may be more difficult to palpate.
A fat-filled vaginal tunic or inguinal lymph node may feel similar to a testicle; however, differentiation is possible with ultrasonography. A normal testicle is hypoechoic to surrounding fat and has a homogeneous medium echotexture with or without a mediastinum testis, which is a mass of connective tissue consistently seen as a 0.2-cm linear hyperechoic structure in the central long axis of the testis.10 Intra-abdominal testicles are usually palpable only when enlarged.
After other external locations have been excluded and the cryptorchid testicle is determined to be intra-abdominal, abdominal radiographs may reveal an enlarged testicle (torsed or cancerous) that appears as a rounded soft tissue mass in the caudal abdomen. Normal-sized intra-abdominal testicles are rarely palpable and are not visible on routine abdominal radiographs.
A recent study showed that ultrasonography can be effective for the detection of cryptorchid testicles, with a sensitivity of 96.6% for abdominal testicles and 100% for subcutaneous testicles.10 Testicular torsion is also readily diagnosed with ultrasonography.11
In cases in which ultrasonography and radiography are not available or the pet owner chooses not to use this method, surgical exploration and removal of the testicle can be pursued.
Both testicles should be removed in cryptorchid patients, even when one testicle is in a normal scrotal location.3 This condition is strongly suspected or known to be genetic in certain dog (eg, toy breeds, boxers, bulldogs) and cat breeds.1,3 In addition, undescended testicles are up to 13 times more likely to become neoplastic than normally located testicles and are more prone to torsion12; both testicles should always be submitted for histopathology. Surgical placement of an ectopic testicle in the scrotum (ie, orchiopexy13) has been reported but is not recommended.
Surgical Removal
Prescrotal Testicles
The testicle should be pushed toward the midline and an incision made through the skin and superficial subcutaneous layer. The spermatic cord and the testicle should be dissected free of surrounding soft tissue and should be double mass ligated. The scrotal testicle should be removed using a standard prescrotal neuter method.
External Inguinal Testicles
If the cryptorchid testicle is palpated in the subcutaneous tissue of the inguinal region, an incision should be made directly over the ectopic testicle to expose and remove it. Because the testicle may be deep in the inguinal fat pad, dissection should be performed carefully to identify and avoid damage to the nearby pudendoepigastric vasculature. The testicle and spermatic cord should be dissected free of surrounding soft tissue and the procedure completed using a standard method.
Testicles Within or Deep to the Inguinal Canal
Inguinal Approach
An inguinal approach may be chosen when the location of the testicle is unknown; most abdominal ectopic testicles and those caught in or just deep to the inguinal canal can be removed with this approach.14 If a spermatic cord extending caudally from the inguinal ring is found during early extra-abdominal dissection, the cord should be dissected, the subcutaneous testicle dissected free of surrounding soft tissue, and a routine closed neuter performed.
Skin should be incised 4 to 6 cm in a longitudinal direction over the inguinal ring area and prominent vaginal process, which is an embryonic outpouching of parietal peritoneum that extends through the inguinal ring. The author prefers to incise slightly lateral to the fatty tissue under the fifth mammary gland to avoid damaging the underlying epigastric vessels. Dissection should be continued down to the inguinal ring and vaginal process; in cryptorchid dogs, the process appears as a small, sausage-shaped pouch-like structure that may be partially filled with fat. Fat and connective tissue from the vaginal process should be dissected and the end of the process grasped with Allis tissue forceps. The vaginal process should be carefully inspected and the inguinal extension of the gubernaculum (Figure 1) identified; this is seen as a thin band of fibrous tissue (2-4–mm thick in dogs, 1-2–mm thick in cats) exiting the inguinal canal and extending from the apex of the vaginal tunic toward the scrotum.


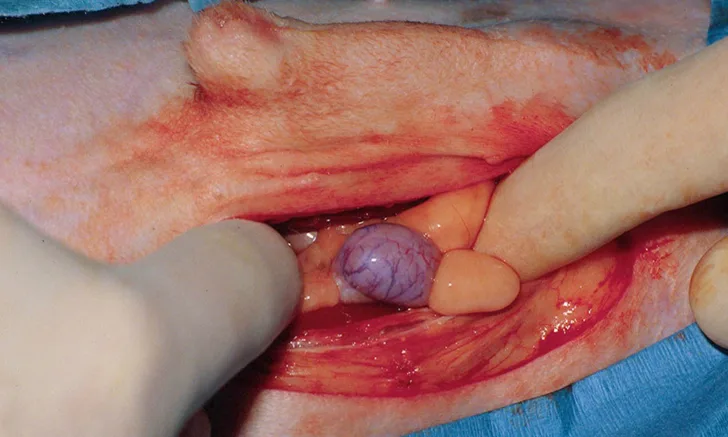
Limited inguinal approach in which the gubernacular extension is grasped and pulled caudally to expose the vaginal process (A; arrow). The vaginal process is incised with continued traction of the gubernaculum (B; arrow), and the connected testicle is exposed (arrowhead). Images courtesy of Journal of the American Veterinary Medical Association
Controlling hemorrhage during this procedure enables isolation of the minute structures (ie, gubernaculum, vaginal tunic).
A small incision into the vaginal process should be made and the interconnected epididymal ligament, ductus deferens, and tail of the epididymis identified. Continued traction should be applied on any of these structures or the gubernacular ligament while the testicle is pulled through the inguinal ring (see Author Insight). The spermatic vessels and ductus can be double-ligated separately after the testicle is exteriorized. If the inguinal rings are enlarged during the procedure, several interrupted sutures can be placed in the external inguinal ring at the cranial aspect while avoiding nearby neurovascular structures.
AUTHOR INSIGHT
In some older dogs (eg, patients with a testicle enlarged due to a tumor), the inguinal ring may need to be enlarged. This can be accomplished by incising the cranial aspect of the external inguinal ring to permit final passage of the ectopic testicle through the canal.
A paramedian approach should be used if no testicle is found, the gubernaculum is not identified, an enlarged testicle cannot be pulled into the subcutaneous space, or a friable gubernacular ligament ruptures during traction, causing the testicle to retract and become lost in the abdominal cavity.
Abdominal Testicles
Ventral Midline Approach
A ventral midline approach can be used if the testicle is enlarged and pathologic. This approach should be selected when a complete abdominal exploration is also necessary, as bilateral intra-abdominal testicles can be readily removed. An incision should be made on the midline from the umbilicus caudal, paramedial, and extended to (at least) the midpoint of the prepuce. The incision should be extended to obtain ideal exposure, allow easy removal of a torsed or enlarged neoplastic testicle, and inspect local lymph nodes and associated pathology.
Paramedian Approach
The paramedian approach is the author’s preferred method for unilateral cryptorchid neuters when the ectopic testicle cannot be located with imaging or palpation, is in the abdomen, or is trapped in the inguinal canal and laparoscopic equipment is unavailable.15 This approach avoids dissection around the prepuce, and the incision is lateral to the epigastric vasculature. Minimal undermining is required; therefore, dead space is minimized. No additional retraction is needed because the dissection plane runs directly from the skin incision to the abdomen. Before entrance is made into the abdomen, the surgeon should proceed to the inguinal ring region to determine whether the testicle can be easily and digitally palpated or whether a spermatic cord can be identified extending caudal to the inguinal ring in the subcutaneous tissue. In these cases, a further caudal incision is needed for the skin and subcutaneous tissue to expose and excise the testicle.
The longitudinal incision should be centered lateral and parallel to the nipple line and midway between the tip of the prepuce and the vaginal process (Figure 2). The skin and subcutaneous tissue should be sharply incised and, before approaching the abdomen, an index finger should be moved along the loose connective tissue plane just superficial to the abdominal fascia. The inguinal ring area should be palpated carefully for a testicle. If a testicle is not found, the index finger should continue to push along the fascia until it is caudal to the inguinal ring and superficial to the pubic bone, then the finger can be swept laterally to identify a spermatic cord. If a spermatic cord is found, the incision should be lengthened caudally and the neuter can be completed.

An incision is made parallel and lateral to the nipple line (and lateral to the course of the caudal superficial epigastric vessel that is faintly visible). The incision extends from the level of the preputial orifice to just cranial to the inguinal ring.
If no cord can be palpated, the testicle is either in the abdomen or, more rarely, stuck in or deep to the inguinal canal. A longitudinal incision should be created just medial to the myofascial line through the external abdominal oblique fascia and continued past the internal abdominal oblique fascia, with blunt spreading between the rectus abdominis muscle fibers (Figure 3). The thin peritoneal layer below should be identified, and the epigastric vessels deep and medial to the incision should be avoided.

Separate fascias of the external and internal abdominal oblique muscles are incised, exposing the fibers of the rectus abdominis.
The surgeon should bluntly puncture and digitally widen the peritoneum; the ectopic testicle usually pops into the field. If no testicle is readily apparent, an index finger can be used to sweep and snare the ductus deferens. If the ductus cannot be isolated, the bladder can be caudally reflected to expose both ductus deferens as they approach the prostate. The respective ductus should be gently pulled to determine if the attached testicle can be pulled into the approach. If this is not successful, the ductus can be judiciously pulled cranially with one hand and the ductus followed to the internal inguinal ring. If the ductus runs into the inguinal ring, the skin incision should be expanded and an inguinal approach should be adopted (Figure 4).

After the fibers of the rectus abdominis muscle are bluntly divided, the testicle is identified and retracted from the abdomen to expose the ductus and testicular vasculature.
The paramedian approach repair is initiated with combined closure of the internal and external abdominal fascia edges in a simple continuous pattern. Subcutaneous and skin layers can be closed routinely.
Avoiding Intraoperative Complications Due to Poor Exposure
A paramedian approach can help avoid inadvertent ureteral avulsion or prostatectomy. To avoid damage to the ureter or prostate, the structure isolated in the caudal abdomen should be confirmed to be a testicle. Aggressive pulling or tissue retraction should be avoided when attempting to expose a cryptorchid testicle. Retraction of a ureter misidentified as a ductus deferens could cause damage or even avulsion. If a spay hook is used to snare the ductus deferens, the tissue connected to the ductus deferens should be carefully inspected. The prostate can be mistaken for a cryptorchid testicle; careful inspection can help avoid this mistake.16 In addition, both the prostate and testicle are connected to the ductus; however, the ductus runs dorsal and medial to the prostate and lateroventral to the testicle. An abdominal testicle is more freely attached and is easily retracted into the field for ligation unless trapped in the inguinal canal (Figure 5). If the testicle is not readily retracted into the field, the ductus can be followed laterally toward the internal inguinal ring. If the ductus runs into the inguinal canal, the inguinal approach can be adopted.

Left paramedian approach to remove a free left abdominal cryptorchid testicle
Laparoscopic Approach
When laparoscopy is available, it provides exceptional visualization for testicle identification and removal and is the author’s preferred method for removing unilateral and bilateral intra-abdominal testicles.
Laparoscopic-Assisted Technique (2-Port)17
A 6-mm cannula should be safely inserted on the midline just caudal to the umbilical scar via a Hasson or Veress needle technique. The abdominal cavity should be insufflated, and a 0-degree rigid laparoscope should be inserted through the cannula. The abdominal cavity should be explored first. If the ductus is followed to the internal inguinal rings, the scope can be removed and the approach converted to inguinal in order to identify and remove the ectopic testicle. If an abdominal testicle is identified (Figure 6), a second 6-mm port should be inserted in a position ventral and slightly lateral to the testicle. The second cannula placement should be directly visualized with the scope. The testicle should be pulled with laparoscopic graspers through the lateral port, which can be expanded to remove an enlarged testicle. The cryptorchid testicle should be routinely ligated and removed outside the abdominal cavity.

A cryptorchid testicle identified adjacent to the urinary bladder with a laparoscope. Image courtesy of Journal of the American Veterinary Medical Association
Single Incision Multiport Technique
The author prefers a single incision laparoscopic surgery (SILS) multiport technique18 for cryptorchid neuter when a minimally invasive approach is elected. This involves a single incision; multiple instruments can be inserted simultaneously for visualization, grasping, retracting, and vessel sealing. Unlike the 2-port technique, the SILS port site does not need to be expanded to remove an enlarged testicle because the port is removed first.
An SILS port should be placed on the ventral midline at the umbilical scar using a Hasson approach. Appropriate-sized cannulas should be inserted in the port and the abdomen insufflated. After exploration with the scope, a grasper can be used to hold and retract the ectopic testicle. A vessel sealing device should be used for hemostasis. If a vessel sealer is not available, the vessels and ductus can be ligated as described with the 2-port technique. While the freed testicle is being grasped, the port should be pulled out of the abdominal wall, and the testicle should be routinely ligated and removed. The incision can then be routinely closed.
Cryptorchid Neuter for Cats
Testicles that are palpable in the subcutaneous tissue should be removed longitudinally by incising directly over the inguinal testicle. Once the testicle is exposed, it should be bluntly dissected and removed after routine ligation of the spermatic cord. In cases in which the testicle cannot be palpated, which is common, a caudal ventral midline approach should be used to incise from the umbilicus to 1-cm cranial to the pubic brim. No prepuce overlies the linea alba in cats, so a simple direct approach can be used.
The midline fascia should be exposed using a sharp, careful dissection of the inguinal fat off the underlying fascia until the inguinal canal area is exposed. The inguinal ring should be inspected for the gubernaculum or spermatic cord. If a spermatic cord is found extending caudally from the ring, blunt dissection should be performed around the spermatic cord and the cord pulled cranially to expose the testicle. In many cases, the testicle may appear as an indistinct, small, soft tissue structure at the terminal end of the spermatic cord; the mass and terminal cord should be removed.
If only the gubernaculum is found extending from the canal, the testicle is either free in the abdomen or caught at the inguinal canal. A midline approach to the abdominal cavity should be adopted, and a finger should be used to sweep and pick up the ductus deferens, which should be gently pulled up and followed until the testicle is found. If the ductus extends to the internal inguinal ring and the testicle cannot be teased into the abdomen for removal, dissection of the external inguinal ring can be performed and the gubernaculum isolated. The gubernaculum should be firmly pulled up until the testicle is dissected from the inguinal ring. The testicle can then be routinely removed.
Postoperative Care & Complications
For all mentioned procedures, the author recommends a peri-incisional block with administration of a prolonged-acting local anesthetic agent (eg, bupivacaine [1 mg/kg]) as the wound is closed. When no contraindications exist, NSAIDs (eg, carprofen, 4.4 mg/kg PO every 24 hours or divided and given every 12 hours, dogs only) should be administered for 3 to 5 days after surgery. Follow-up on the biopsy results and consultation with the owner regarding further examinations or diagnostics may be needed. The incision site should be monitored for local signs of ensuing seroma, infection, or dehiscence. An Elizabethan collar may be needed to prevent self-trauma. The patient can resume routine activity following suture removal.
Complications after cryptorchidectomy are uncommon, and most are local and self-limiting. Serious complications are rare and include dehiscence, hemorrhage from insecure pedicle ligation, inadvertent ureteral avulsion or ligation, and inadvertent prostatectomy.