Palliative Management of Cancer Pain in a Geriatric Cat
Beatriz P. Monteiro, DVM, University of Montreal
Paulo V. Steagall, DVM, MS, PhD, DACVAA, Université de Montréal, Quebec, Canada

Luna, a 15-year-old, 8.6-lb (3.7-kg), spayed domestic shorthair cat with stable International Renal Interest Society stage 2 chronic kidney disease (CKD), was presented for evaluation of an enlarged right rostral mandible, decreased appetite, halitosis, and dysphagia of approximately a month’s duration (Figure 1). The owners also reported recent changes in behavior: Luna had become irritable and could no longer jump onto windowsills.
Physical Examination
On presentation, Luna was quiet and shy. Vital parameters were within normal limits (temperature, 100.8°F [38.2°C]; pulse, 160 bpm; respiratory rate, 36 breaths per min). She was subclinically dehydrated (5%), and her hair coat was greasy. The right submandibular lymph node was enlarged. BCS was 3/9, which was similar to previous visits, with apparently stable body weight. Systolic blood pressure was 140 mm Hg (reference range, <150 mm Hg). Because Luna refused to walk, mobility could not be assessed.
Oral pain was assessed through gentle palpation of the mandible. Luna showed signs of hyperalgesia (ie, increased pain sensation to a painful stimuli) and clear avoidance of palpation while hissing at the clinician. Because osteoarthritis (OA) was suspected, OA-related pain was assessed using the Client Specific Outcome Measures instrument (see Suggested Reading),1 which consisted of choosing and scoring 3 activities that were specific to Luna (ie, jumping onto the kitchen’s window sill in the morning, using the litter box after breakfast, jumping onto the bed in the evening). Luna performed these activities with severe, mild, and moderate difficulty, respectively. Although there is currently no validated instrument to assess quality of life that is freely available to veterinarians, a general quality-of-life assessment was performed by evaluating Luna’s ability to perform daily activities, appetite and grooming habits, and social interactions and temperament.2,3 Because Luna was showing progressively decreased levels of activity and socialization, it was determined that her quality of life was moderately affected.
CBC and serum chemistry profile results revealed mild anemia (hematocrit, 25%; reference range, 28%-47%) and elevated BUN (42.6 mg/dL; reference range, 11.5-30.2 mg/dL) and creatinine (2 mg/dL; reference range, 0.4-1.9 mg/dL) levels. Urine specific gravity was 1.029 (reference range, ≥1.035), symmetric dimethylarginine was 15 μg/dL (reference range, 0-14 μg/dL), and total thyroxine was 1.6 μg/dL (reference range, 1.0-4.4 μg/dL).
Diagnosis
Luna was anesthetized for additional diagnostics. Premedication was administered intramuscularly with a combination of acepromazine (0.02 mg/kg) and buprenorphine (0.02 mg/kg). Thoracic radiography and abdominal ultrasonography were performed with the patient under sedation and revealed no evidence of metastasis. Approximately an hour after premedication, general anesthesia was induced with propofol (5 mg/kg IV) and maintained with isoflurane (1.2%-1.3% expired concentration delivered in 100% oxygen using a nonrebreathing circuit). Intravenous fluids (3 mL/kg/hr) were also administered. A firm mass (1.2 × 2 cm) was identified on the right rostral mandible. Oral radiographs revealed marked osteolysis and periosteal proliferation. An inferior alveolar (mandibular) nerve block was performed using bupivacaine 0.5% (see Local Anesthetic Technique for Nerve Blocks). An incisional biopsy was performed at the junction of normal and abnormal tissues and submitted for histopathology. No attempts were made to surgically remove the mass, as the owners did not want to perform any invasive procedures and wished to only confirm diagnosis. Histopathology results were consistent with squamous cell carcinoma.
LOCAL ANESTHETIC TECHNIQUE FOR NERVE BLOCKS
For local anesthetic techniques of the oral cavity, generally, a maximum bupivacaine dose of 2 mg/kg is calculated, and the total volume is divided among all the local blocks to be performed; in Luna’s case, because only the inferior alveolar (mandibular) nerve block was performed, 0.3 mL of bupivacaine 0.5% was used. The inferior alveolar foramen can be located on the medial side of the mandible approximately halfway between the angular process of the mandible and the last molar tooth. Although the foramen can be difficult to palpate in cats, the block can often still be performed successfully using 2 imaginary lines to locate the mandibular foramen (ie, a line perpendicular to the lateral canthus of the eye can be crossed with another line that divides the dorsal and ventral teeth arcade). The ventral teeth arcade is parallel to the ventral portion of the mandible. The injection point should be located at the intersection of these 2 lines, and the needle should be inserted perpendicular to the ventral margin of the mandible using an extraoral approach (Figure 2). The inferior alveolar (mandibular) nerve block produces anesthesia of the mandible, including the teeth, lower lip, part of the tongue, and hard and soft tissues.10
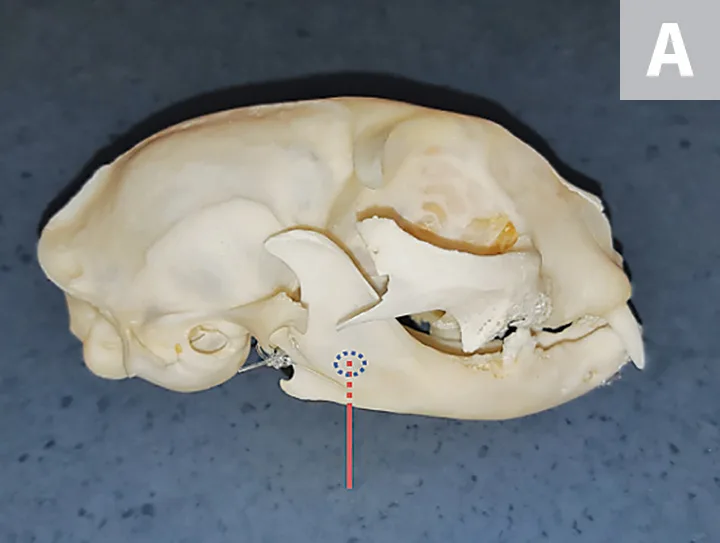
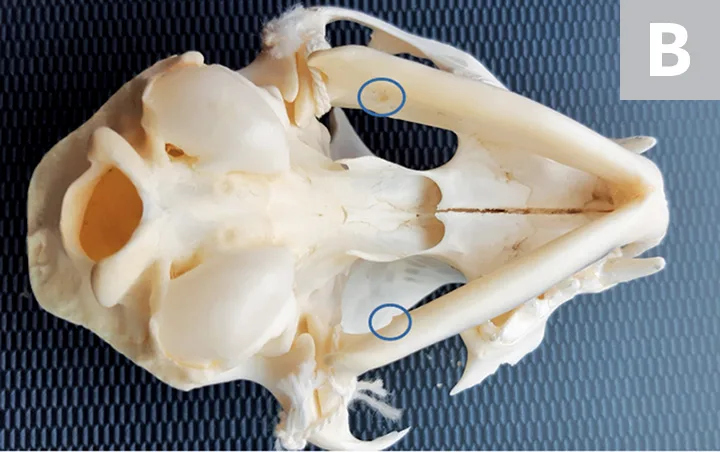
Right lateral (A) and ventrodorsal (B) views of a feline skull to demonstrate the inferior alveolar (mandibular) nerve block technique. The technique should be performed using 27- to 30-gauge, 12- to 16-mm long needles, and a 1-mL syringe. The area of injection of the local anesthetic is indicated by the dotted blue circle. For the extraoral approach, the needle (represented by the red line) should be inserted perpendicular to the ventral margin of the mandible, with the bevel of the needle directed toward the medial aspect of the mandible. The local anesthetic should be injected close to the inferior alveolar foramen on the medial aspect of the mandible (solid blue circles). Prior to injection, aspiration should be performed to confirm that no intravascular injections are being performed. The local anesthetic should be injected slowly, and no resistance should be felt.
DIAGNOSIS:
SQUAMOUS CELL CARCINOMA
Treatment & Long-Term Management
Anesthesia & Acute Perioperative Analgesia
Opioids are safe at clinically acceptable dosages and are excellent analgesics.4 The combination of opioids and acepromazine reduces inhalant anesthetic requirements. Locoregional anesthesia with bupivacaine provides pain relief by blocking sodium channels and the consequent production and transmission of nociceptive stimuli (ie, pain transduction and transmission). Analgesia lasts approximately 6 hours with locoregional bupivacaine.
Luna was hospitalized for 36 hours and maintained on fluid therapy. Pain was assessed every hour for the first 8 hours and every 6 hours thereafter using the Glasgow Composite Measure Pain Scale, which includes evaluation of the cat’s behavior and facial expressions while undisturbed.5 A pain scale score equal to or higher than 5 (out of 20) is the recommended cut-off score for intervention (eg, with buprenorphine [0.02 mg/kg IV q6h]). During pain assessment 4 hours after recovery from anesthesia, Luna was tense and crouched, with facial expressions indicative of pain, based on ear position and muzzle shape; pain score was 7/20. Thus, buprenorphine (0.02 mg/kg IV q6h) was administered. In addition, Luna exhibited a normal appetite when offered soft food, suggesting that the previously reported decreased appetite had been due to oral pain, which was attenuated by analgesic management.
The owners opted for palliative analgesic treatment (see Treatment at a Glance), with the aim of improving quality of life. Treatment of cancer was declined after a thorough discussion.
TREATMENT AT A GLANCE
Chronic pain can be managed on an outpatient basis through both pharmacologic and nonpharmacologic means.
Pharmacologic therapy
For Luna, this included robenacoxib (1 mg/kg PO q24h) and gabapentin (10 mg/kg PO q12h). Tramadol (3 mg/kg PO q12h11) or amitriptyline (10 mg PO q24h) could also have been added to this patient’s analgesic protocol.
Nonpharmacologic management
Environmental enrichment tailored to the patient’s needs. In Luna’s case, this included the addition of scratch posts, toys, and condos; steps so she could have access to windows; play sessions (15-20 minutes of access to the backyard under supervision twice daily); brushing (10-minute sessions twice daily as tolerated); and administration of soft food.
Nonpharmacologic therapies might also include acupuncture and/or nutraceuticals (eg, fish oil or green-lipped mussel extract, glucosamine/chondroitin sulfate, polysulfated glycosaminoglycan [extra-label]).
Long-term chronic pain management should include treatment of breakthrough pain (eg, administering buprenorphine when oral medications and other treatments are not controlling the pain).2
Pain Management & Palliative Care
Luna’s potential sources of pain included cancer pain affecting the oral cavity and bone, as well as pain associated with OA, resulting in mixed inflammatory and neuropathic pain. Therapy was planned using a mechanism-based approach (ie, analgesics to counteract inflammatory and neuropathic pain mechanisms). Luna was discharged on long-term medication, including robenacoxib (1 mg/kg PO q24h [see Extra-Label Drug Use]) and gabapentin (10 mg/kg PO q12h). NSAIDs are excellent analgesics for inflammatory pain but are normally contraindicated in cats with CKD; however, recent research has suggested that NSAIDs may be safely administered long-term in cats with stable CKD.6,7 The decision to initiate NSAID therapy in cats with CKD, however, should be made on a case-by-case basis, and the risks and benefits should be carefully assessed.8 In Luna’s case, the benefits of NSAID therapy were determined to outweigh the risks, particularly because proper nutrition and hydration were being maintained. Gabapentin blocks Ca<sup+2sup> channels and reduces neuronal excitability, and this drug has been shown to provide analgesia in cats with OA and is indicated in conditions that cause neuropathic pain.9
Nonpharmacologic therapy in the form of environmental enrichment was also initiated and included play sessions (15-20 minutes of access to the backyard under supervision twice daily), brushing (10-minute sessions twice daily according to Luna’s preference), and providing scratching posts, homemade toys and condos, and steps to give Luna access to windows. Other nonpharmacologic treatment modalities could include acupuncture and/or nutraceuticals (eg, fish oil or green-lipped mussel extract, glucosamine/chondroitin sulfate, polysulfated glycosaminoglycan [extra-label]). Long-term chronic pain management should include treatment of breakthrough pain (eg, administering buprenorphine when oral medications and other treatments are not controlling pain).2
Luna’s needs were approached from a welfare perspective to provide optimal pain management using pharmacologic and nonpharmacologic options.2,3
EXTRA-LABEL DRUG USE
Clinicians are advised to check local regulations of NSAID administration in their country of practice. For example, in Canada, robenacoxib can be administered once daily for the treatment of musculoskeletal disorders, and the duration of treatment can be decided on an individual basis12; however, in the United States, this drug is only labeled for administration for up to 3 days.13 If extra-label administration is performed, owners should be made aware and perhaps sign a written consent form.
Prognosis & Outcome
Luna’s prognosis was guarded to poor. Recheck visits were performed monthly. Despite pain management, disease was progressive and resulted in pathologic mandibular fractures. Luna’s quality of life could no longer be maintained as an outpatient, and she was euthanized 8 weeks after presentation (see Take-Home Messages).
TAKE-HOME MESSAGES
Oral and bone tumors cause severe pain, which can be controlled using a multimodal pharmacologic and nonpharmacologic approach.
Pain in cancer patients is multifactorial and can originate from the tumor itself, diagnostic procedures, therapies, metastatic disease, and/or concomitant painful conditions.
Owners should be involved in the treatment plan and management of chronic pain by administering analgesics and providing nonpharmacologic therapies.
Cancer pain may become refractory to treatment as disease progresses, and pain management may no longer be achievable on an outpatient basis, requiring hospitalization.
Euthanasia should be considered for cats with severe chronic pain and/or poor quality of life. Decisions should be made on a case-by-case basis.
CKD = chronic kidney disease, OA = osteoarthritis