Smartphone Technology in Clinical Ophthalmology
Lucien V. Vallone, DVM, DACVO, Texas A&M University

A miniature schnauzer presented for red eye. This representative image of poor photographic technique was taken from a close working distance, but shadowing obscures details of the ocular surface from being perceived.
We sat down with Dr. Vallone to further discuss how smartphones can be used in ophthalmic examinations. Listen to his episode of Clinician's Brief: The Podcast here.
Advancing smartphone technology is allowing clinicians to capture high-resolution photos and videos and facilitate convenient means of medical examination, documentation, and subsequent consultation in multiple disciplines, without the need for special techniques or accessory products.1
Reports of smartphone photography and examination techniques in animals are limited mostly to individual descriptions of smartphone camera adapters used for fundoscopy.2-4 Successful fundus imaging has been achieved using such equipment; however, this incurs additional cost and equipment is often limited to specific smartphone models. The following outlines techniques for fundus and anterior segment imaging that predominantly do not require the purchase of accessory equipment.5,6
Maximizing Smartphone Camera Features
It is important to capture as much detail as possible when documenting ophthalmologic disorders. Examiners should maximize intrinsic smartphone camera features that can be adjusted to create adequately magnified, focused, and illuminated images of the eye. To achieve this, the smartphone camera should be brought to the minimum focusing distance (ie, the closest point at which a focused image is still maintained) before capturing the image. If available, optical zoom should be enabled to capture enhanced (typically ≤ 2×) magnification without losing image quality. Image quality (ie, resolution) is degraded when digital zoom—for most smartphones, typically anything > 2× magnification—is used. Modern 4K image resolution (ie, 3840 × 2160 pixels) allows smartphone photographers to significantly crop and enlarge photographs while still maintaining high-definition images capable of being printed or published at ≥300 pixels per inch.
Shadowing and underexposure of the ocular surface and intraocular structures are common problems with smartphone photography, often yielding images of poor diagnostic quality (Figure 1). Close working distances, delayed flash, and patient movements all make smartphone flash photography of the eye difficult. These obstacles can be overcome and shadowing and underexposure avoided by enabling the continuous flash in the camera’s video mode (see Continuous Flash Technique). When capturing images in this manner, it is often helpful to direct light into the pupil so a fundic/tapetal reflection is generated (Figure 2). External illumination (eg, overhead surgical lamp, transilluminator, penlight) can also be used to reduce shadowing of the eye (Figure 3).

A horse evaluated for recurrence of ocular squamous cell carcinoma. The image was captured as a screenshot of a continuous-flash video in which light had been directed toward the pupil. This technique provides adequate illumination of both the intraocular and extraocular structures.
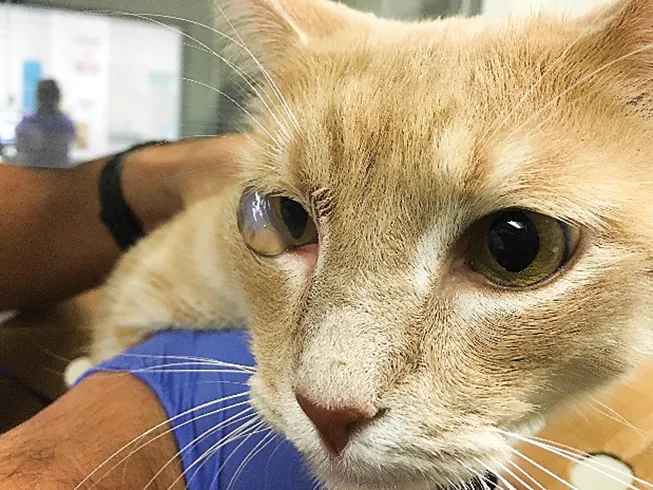
A close working distance and overhead illumination of this patient’s right eye help avoid shadowing and demonstrate the distinctive clinical appearance of feline eruptive bullous keratopathy (ie, corneal hydrops).
Continuous Flash Technique
This technique helps improve illumination of the eye when imaging the anterior segment and/or adnexa or performing direct or indirect fundoscopy. The continuous flash technique can be used by following these steps:
The flash should be dimmed, either by using a camera app (eg, FiLMiC Pro, MAVIS, MoviePro, Cinema FV-5) or by applying 1 to 3 layers of white medical tape to act as a diffuser.
Although the LED flash of one common smartphone model has been determined to be safe in humans,16 it is important to recognize that the smartphone flash is extremely bright and, as such, may cause significant patient discomfort, potentially leading to resistance or lack of cooperation, particularly when used in a close working distance.
The camera application should be toggled to video mode, and the camera’s flash should be enabled to run continuously.
The examiner should then capture video, attempting to record all representative features of the subject.
Still frames can be captured in real time by taking photographs while in video mode or, retrospectively, by reviewing the video and taking screenshots.
Macro Photography
The unaided human eye and the unassisted smartphone are both insufficient when screening for many of the most common ocular pathologies encountered in small animal practice. These pathologies are too small to be easily observed without visual assistance but are crucial to the accurate diagnosis and treatment of many ocular disorders. Thus, in these circumstances, achieving magnification beyond optical zoom is required; numerous, inexpensive smartphone accessory products can help accomplish this. For example, macro lens smartphone camera attachments can be used to considerably enhance photographic and video magnification.
The author routinely uses a commercial universal smartphone macro lens attachment (ie, Easy-Macro) that provides 4× magnification via a small plastic lens embedded in a rubber band. The rubber band wraps around the body of the smartphone, and the lens is situated in front of the camera (Figure 4). Once the lens attachment is affixed to the smartphone camera lens, the camera application should be toggled to video mode. The focal point is dramatically shortened with this technique, requiring the examiner to bring the phone 1 to 2 cm from the eye until a focused image can be observed on the screen. Further magnification can be achieved by enlarging and cropping these still images (Figure 5).

FIGURE 4
Mounted appearance of a macro lens (Easy-Macro) to an iPhone XS Max. The flash component of many smartphones is aligned horizontally, rather than vertically, as shown here; this may obscure the flash and require the examiner to provide independent illumination (eg, penlight) to the eye.
Direct Fundoscopy
Most smartphones are capable of imaging the fundus without modifying the phone with accessory attachments (see Ideal Smartphones for Direct Fundoscopy). The technique is simple to perform, and images can be obtained at very high quality. The camera application should be toggled to video mode and the flash should be set to run continuously (see Continuous Flash Technique). The camera lens should be brought within 1 to 2 cm of the patient’s pupil until a focused image is observed on the screen. The central and peripheral fundus should be scanned and the examination completed.
Ideal Smartphones for Direct Fundoscopy
There are 2 important factors to consider when selecting a smartphone that is ideal for direct fundoscopy:
Whether the rear-facing camera lens is located centrally or peripherally on the back of the smartphone. Due to the requisite proximity and alignment of the camera lens to the eye and pupil, respectively, the direct fundoscopy technique is most practical for smartphones with peripherally positioned cameras (eg, iPhones, Google Pixel). Smartphones with centrally positioned rear-facing cameras (eg, Samsung Galaxy Note, LG) can be difficult to align with the pupil of dogs and cats, as the peripheral body of the smartphone will encounter the patient’s muzzle before camera alignment can be achieved. With a peripherally positioned rear-facing camera, the patient’s muzzle does not interfere with this alignment. Both eyes can be imaged directly with these types of smartphones by rotating the phone so the rear-facing camera is positioned medially near the muzzle. This technique can take time and patience, particularly with larger smartphone models, which can be difficult to handle.
The smartphone’s flash position relative to the camera lens. The camera flash should ideally be positioned as close to the camera lens as possible to reduce shadowing from the iris (Figure 6). The camera and flash position vary among models (range, ≈5-25 mm), making some smartphones better suited for direct fundoscopy than others. Assessing the distance between the lens and flash is less intuitive when evaluating smartphones with dual-camera designs (eg, iPhone 7 Plus, iPhone 8 Plus, iPhone X). Dual-camera smartphones typically possess a traditional wide-angle lens and an added telephoto lens, which does not support the techniques outlined in this article. The wide-angle lens is well-suited for direct fundoscopy and, in iPhone models, is located closer to the top left corner of the smartphone, regardless of vertical or horizontal dual-lens orientation. The iPhone X may be better suited for direct fundoscopy as compared with the iPhone 7 Plus and iPhone 8 Plus, as the flash is located closer to the wide-angle lens.

With direct fundoscopy, shadowing occurs most often when the flash is positioned relatively far from the camera lens, as shown in these images of an Australian shepherd dog (A) and an alpaca (B) obtained using an iPhone 8 Plus.
Autofocus & Autoexposure
Default settings on most smartphones automatically adjust the focus and exposure settings to enhance photo quality. This does not always benefit the examiner when performing direct smartphone fundoscopy, as lens opacities and tapetal reflections can interfere with autofocus and autoexposure adjustments, respectively. To mitigate this issue, the examiner can lock these settings; to do so on iPhones, the examiner can press and hold the screen over the subject when in camera/video mode and when the camera is focused on an object several paces away (eg, the far wall of an examination room).
Pupil Constriction
Although direct fundoscopy is possible in non-dilated patients, ocular examination can be improved considerably with the use of a topical mydriatic (eg, tropicamide). However, examiners can still capture fundus images in a nonpharmacologically dilated patient by reducing the light in the examination room, covering the camera flash with additional filters (eg, white medical tape), and/or downloading an accessory camera smartphone application that facilitates manual adjustments to the flash intensity (eg, FiLMiC Pro).3-5
Indirect Fundoscopy
For indirect fundoscopy, smartphones can be used as a light source while simultaneously serving as a recording device. This technique is applicable to nearly all smartphones capable of running a continuous flash while video mode is selected (see Continuous Flash Technique) and requires a condensing lens be positioned over the eye to create an image that appears inverted and transposed.
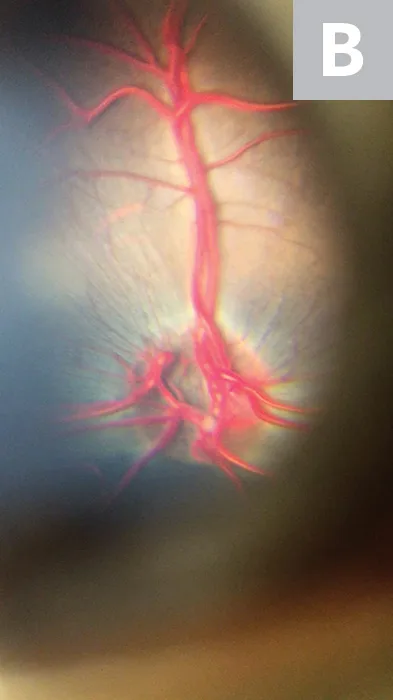
The indirect technique requires an assistant to restrain the patient and, ideally, to open the patient’s eyelids. The examiner should position a condensing lens in front of the eye with one hand and the smartphone between the lens and the examiner’s eye with the other. The lens should be moved into a position that brings a virtual image of the fundus into focus (Figure 7). This technique is more difficult than the direct technique but can be used to successfully view and record the fundus in many circumstances in which the direct technique fails. In particular, the indirect technique is better suited to image the fundus when the pupil is poorly dilated and also forms better fundus images when lens opacity is present (Figure 8). Furthermore, the indirect technique generates images with a much wider field of view as compared with the direct technique and allows the examiner to evaluate peripheral aspects of the fundus with greater ease.
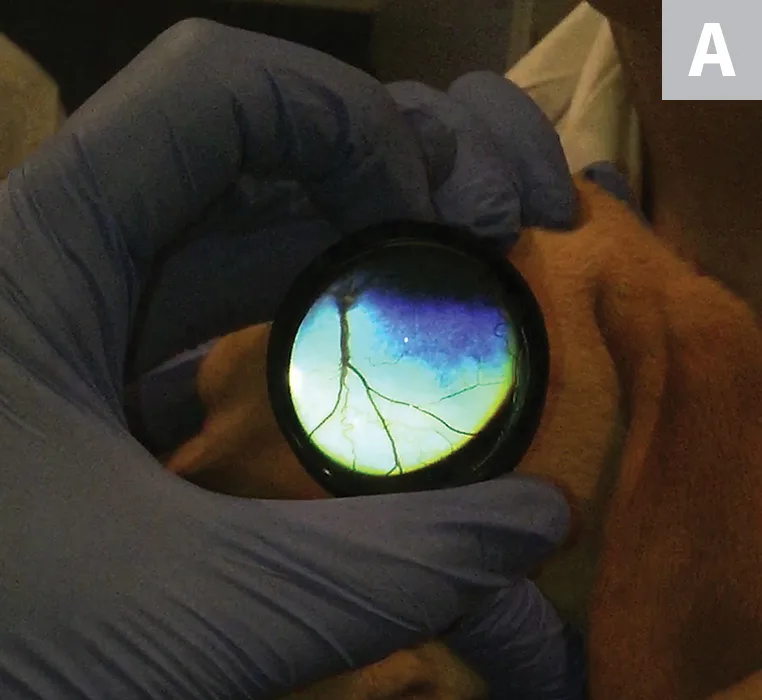
FIGURE 7A
Representative images from a nonvisual Labrador retriever puppy evaluated with the indirect technique (A). Cropped images (B) demonstrate optic nerve hypoplasia. The optic nerve is dark and very small as compared with a normal, well-myelinated optic nerve, as shown in Figures 8B and 8C.
Smartphone Technology in Veterinary Education
Teaching clinical ophthalmology,7 particularly fundoscopy, is a well-documented challenge in human8 and veterinary9 medical training programs that has led to decreased confidence in practitioners’ ability to diagnose and manage common and potentially vision-threatening ophthalmologic disorders.10 Numerous methods of improving fundoscopy training have been published, including the use of novel software programs,11 augmented reality simulators,12 and inexpensive fundus-simulating models.9 Similarly, the acquisition and interpretation of fundus photography has recently been shown to enhance the examiner experience, lesion identification, and long-term retention of fundoscopy skills among medical trainees.13,14 Smartphones are being used with these educational targets in mind. In a study, medical students who used an FDA-approved smartphone adapter to image the fundus reported greater confidence and proficiency when identifying normal fundus structures as compared with settings in which the direct ophthalmoscope was used.15
The use of smartphones for teaching ophthalmoscopy skills in veterinary medical training programs has tremendous potential and deserves further research. In this author’s experience, students and practitioners who have previously been intimidated by the ophthalmologic examination typically find that smartphone imaging techniques make the ophthalmologic examination more accessible.
Conclusion
Smartphones are versatile in medical settings and capable of augmenting the ophthalmologic examination in clinical practice. In the near future, veterinary medicine may see an expansion of teleophthalmology in the broader context of telehealth. Smartphones will be integral to this development. By incorporating some of the imaging techniques outlined above and using basic means of smartphone communication while adhering to prevailing state jurisprudence privacy statutes, veterinary practitioners may find themselves better equipped to triage and monitor ophthalmologic disorders, consult with specialists, and educate pet owners.