Retinal Detachment
Caryn Plummer, DVM, DACVO, University of Florida


External photograph of a terrier dog with RD. The retinal vessels are visible even from a distance, indicating that the retina has detached and come anteriorly within the vitreal chamber.
Retinal detachments (RDs) may develop secondary to a variety of systemic and/or local (ocular) conditions.
In the normal state, the retina sits directly adjacent to the concave contour of the posterior globe to receive oxygen and nutrients from the choroid, with which it is intimately associated. When the retina detaches, it floats anteriorly within the vitreal chamber and is evident as a thin grey veil with visible vasculature (Figures 1 and 2).
Retinal detachment may be unilateral or bilateral. If the cause is related to a systemic condition or a congenital or inherited ocular condition, both eyes are likely to be affected to some degree, although perhaps asymmetrically or sequentially. Local disease, such as unilateral trauma, cataract, or intraocular neoplasia, will typically only result in detachment in the affected eye.

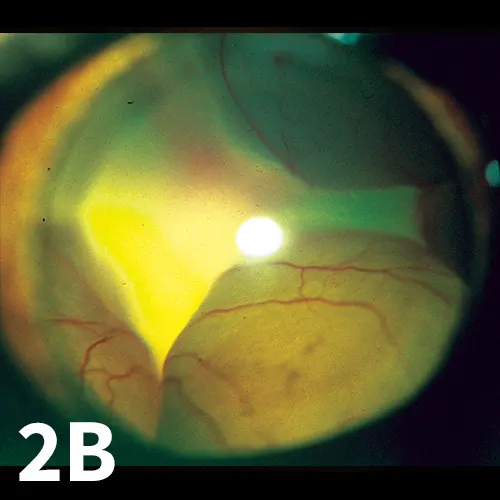
Bullous RD in cats secondary to systemic hypertension. Note the vessels are in different planes of focus. A focal intraretinal hemorrhage is present (A). Images were obtained without use of an ophthalmoscopy lens.
Clinical Signs
RD is usually associated with mydriasis and incomplete or absent pupillary light reflexes. If a detachment is complete, the affected eye will be blind. Some sight may be retained with partial detachment. Accompanying uveitis or intraocular hemorrhage may also be present, particularly if the underlying cause is vascular (eg, systemic hypertension) or traumatic.
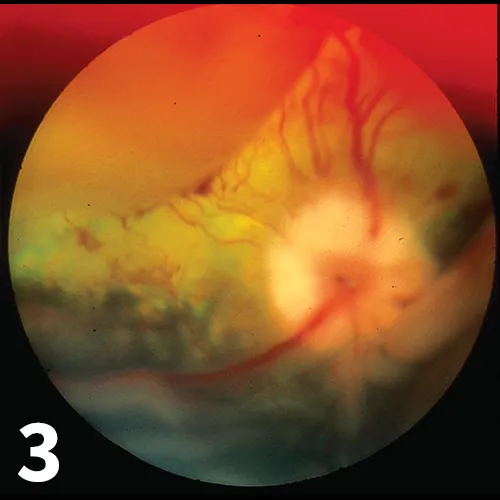
Photograph of the fundus of a dog utilizing a condensing lens for indirect ophthalmoscopy. RD and intra- and subretinal hemorrhage are demonstrated. Note the different planes of focus, the indistinct margins of blood vessels, and the prominent dorsal and ventral partial detachments. These conditions were secondary to acute kidney disease and systemic hypertension in this patient.
Diagnosis
Diagnosis of RD is made during a thorough ophthalmic examination that includes either direct or indirect ophthalmoscopy. RD will appear either as a thin grey veil of tissue with visible blood vessels or as a hyporeflective section of the fundus with indistinct or fuzzy margins on ophthalmoscopy. Retinal blood vessels may be observed in different planes of focus depending on how far forward they have been displaced (Figure 3).
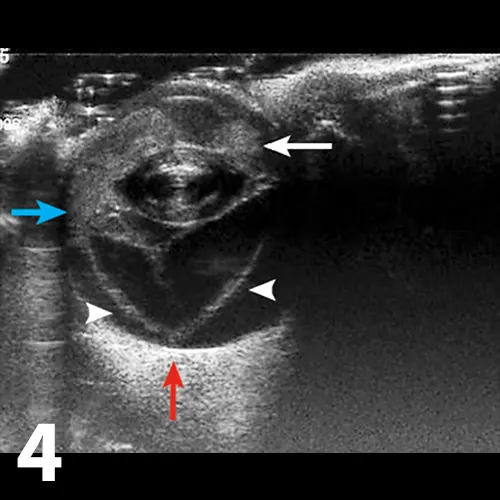
Ultrasonographic image of an eye, with the cornea oriented to the top of the image. The anterior chamber is filled with hyperechoic material, consistent with hemorrhage and fibrin (white arrow) that were evident on examination. The retina is detached (arrowheads) and is forming the classic seagull sign; 2 hyperechoic linear structures representing the retina (arrowheads) within the vitreal chamber, attached at the ora ciliaris retinae (blue arrow) and the optic nerve (red arrow).
Ocular ultrasonography is necessary if the posterior segment of the eye cannot be visualized because of corneal opacity, debris in the anterior chamber associated with uveitis, or cataract; ultrasonography may show a thin, linear hyperechoic structure protruding into the vitreal chamber. Most commonly, the retina will remain attached at the optic nerve and ora ciliaris retinae, which is where the ciliary body transitions into choroid and the peripheral retina begins (Figure 4). This will cause a gullwing appearance, or “seagull” sign, on ultrasonography, but partial detachments or disinsertions (tearing of the retina in addition to detachment) will not show the classic seagull sign.
When a patient has acute vision loss and RD, investigation of the underlying cause should include measurement of systolic blood pressure, a complete physical examination, and a minimum database consisting of a CBC, serum chemistry panel, and urinalysis. RD may result from panuveitis secondary to infectious diseases (including fungal, bacterial or rickettsial causes), trauma, neoplasia (ocular or systemic), congenital ocular diseases (eg, Collie eye anomaly), or cataracts.
Treatment
Treatment depends on the cause of RD. If the RD is a result of systemic hypertension, prompt therapy with systemic antihypertensive agents (eg, calcium channel blockers, angiotensinconverting enzyme [ACE] inhibitors) is indicated. As blood pressure normalizes, the retina will often return to its normal or near-normal anatomic position.
If detachment is secondary to an inflammatory or autoimmune condition, treatment of the primary problem and the associated inflammation (typically systemic corticosteroids) may affect improvement. RD associated with primary ocular disease (congenital anomalies such as retinal dysplasia or lenticular disease such as cataract) may be difficult to treat; referral to a veterinary ophthalmologist for evaluation for reattachment surgery may be indicated.
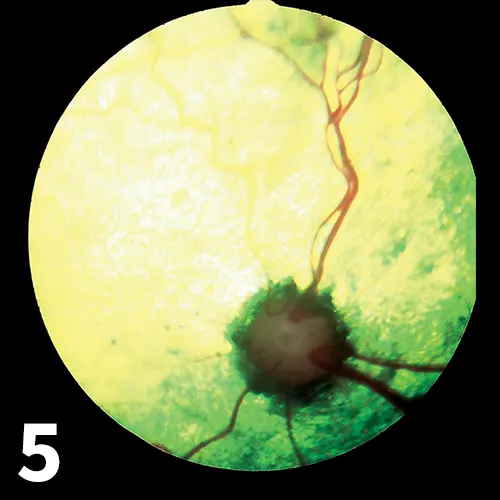
Retinal degeneration following reattachment in a hypertensive cat. Note the hyperreflective tapetum, mild retinal vessel attenuation, and optic nerve atrophy and pallor.
Prognosis
The prognosis for regaining vision following retinal detachment is usually guarded- to-poor. If the RD is caused by systemic hypertension that is corrected promptly, reattachment may occur and vision may be restored. However, if the detachment is chronic or has been associated with extensive retinal or intraocular inflammation, return of sight is unlikely. Retinal degeneration is a common sequela to RD even if physical reattachment occurs (Figure 5).