Recurrent Skin Infection: Treatment & Owner Education

A 66-lb castrated golden retriever-mixed breed was presented for recurrent skin infection of 2 years’ duration involving the right lateral neck.
History
The initial lesions appeared shortly after treatment for unilateral Pseudomonas spp infection of the right ear; this was treated for 10 days with a compounded ear cleaner (enrofloxacin, glucocorticoids) and enrofloxacin (6 mg/kg PO q24h). Owner description of the initial presentation was compatible with pyotraumatic dermatitis. The owners clipped the hair surrounding the lesion and treated it with triple antibiotic ointment. When the lesion did not resolve, veterinary care was sought and the lesion was treated with consecutive 10-day treatment regimens of cephalexin at 30 mg/kg PO q12h, cefpodoxime at 5 mg/kg PO q24h, clindamycin at 22 mg/kg PO q12h, and ciprofloxacin at 10 mg/kg PO q12h. The patient had no other history of dermatologic problems, received a balanced diet, and was on year-round flea and tick control.
Related Article: 5 Things Veterinarians Should Know About Methicillin-Resitant Infections
Physical Examination
Except for the skin, the physical examination was unremarkable. Initial examination revealed scales and erythema on the right lateral neck. Clipping of the hair coat revealed additional skin lesions on the right lateral face and neck (See Figure 1 above, Lesions after the hair coat was clipped. Note the crusted papular eruption and spreading epidermal collarettes). The clinical lesions were compatible with a superficial follicular disease, likely pyoderma based on crusted papules and spreading epidermal collarettes. Pyoderma on the face and neck is common in retrievers with lesions often developing into areas of deep pyoderma (ie, deep pyotraumatic dermatitis).
Related Article: Recurrent Pyoderma in a Golden Retriever
Laboratory Results
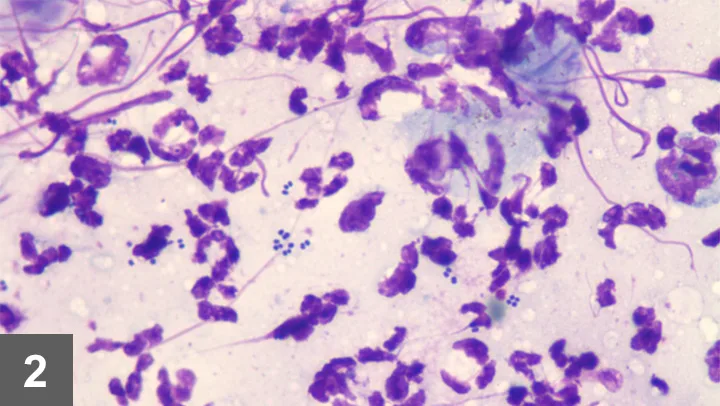
Skin scrapings and hair trichograms were negative for Demodex spp mites. Microscopic cytology samples of the lesions (See Figure 2, Cytology sample from the lesions. Note numerous bacteria and neutrophils.) were obtained. Bacterial culture and sensitivity tests using minimum inhibitory concentrations were performed (See Table below).
ASK YOURSELF...
In this case, which of the following is important owner communication?A. Stress difference between types of resistant infectionB. Treatment optionsC. Treating recurrenceD. Home care and zoonotic riskE. All of the above
NI = no interpretation available,R = resistant
CORRECT ANSWERE. All of the above
Bacterial culture and sensitivity testing revealed methicillin-resistant Staphylococcus pseudintermedius (MRSP) susceptible to gentamicin, rifampin, amikacin, and vancomycin.
Related Article: Tail Mass in a Dog
Stress Differences Between MRSA & MRSPThe owner, a nurse, was familiar with methicillin-resistant Staphylococcus aureus (MRSA) infections and aware that recurrent bacterial pyoderma caused by MRSP is increasingly common in veterinary medicine.1 Because there was concern that this may have been MRSA, it was appropriate to confirm with the microbiology laboratory that the infection was MRSP, not MRSA.
Many laboratories report results as S intermedius group (SIG) or S pseudintermedius, as the latter is the most common canine pathogen. The SIG group consists of S pseudintermedius, S intermedius, and S delphini, and absolute identification requires molecular testing.2 S aureus can be isolated in 12% to 14% of healthy dogs but most likely presents transient colonization or contamination from humans, often when owners are healthcare workers.3
Treatment Options

Treatment for this patient was difficult because the condition was a multidrug-resistant MRSP and oral systemic antibiotics were not an option. Although the MRSP was not resistant to rifampin, which is common, it was not considered an option, as there was no suitable antibiotic to use in conjunction and its use as a single therapy is not recommended.4 Treatment involved whole-body bathing with a chlorhexidine shampoo 3 times weekly and topical mupirocin ointment q12h. Whole-body shampoo therapy was recommended because, although the lesions appeared focal, colonization was generalized and typically may persist after resolution of MRSP pyoderma5; 3 times weekly bathing has been efficacious as sole therapy.6
A recent in vitro study showed chlorhexidine, benzoyl peroxide, and ethyl lactate to be efficacious against MRSP; however, chlorhexidine-containing products were found to be superior.7 Focal topical therapy options included mupirocin ointment, benzoyl peroxide gel, fusidic acid, and nisin1; in this case, q12h application of 2% chlorhexidine gluconate spray was effective for treating MRSP, even though the infection was generalized.
Treating Recurrent InfectionRecurrent infection implies an underlying trigger. Common triggers for recurrent bacterial infection include undiagnosed underlying skin disease (eg, allergic skin disease, primary disorder of keratinization, endocrine disorder), lack of recognition or treatment of concurrent infections (eg, Malassezia overgrowth), or failure of initial treatment (eg, antibiotic selection, duration of treatment). In this patient, there was sporadic recurrence despite aggressive search for an underlying cause. Ultimately, outbreaks were prevented with once- or twice-weekly whole body bathing and twice-weekly application of 2% chlorhexidine gluconate solution as a whole body spray.
MRSA = methicillin-resistant Staphylococcus aureus, MRSP = methicillin-resistant Staphylococcus pseudintermedius, SIG = Staphylococcus intermedius group, tris-EDTA = trisaminomethane ethylenediaminetetraacetic acid
Home Care & Zoonotic RiskThis owner had numerous questions about screening other pets, decolonizing pets, risk for transmission to children, and home hygiene. Because S pseudintermedius evolved to survive on pets, it is difficult (perhaps impossible) to decolonize them.
Overall, MRSP has low zoonotic risk.3 S pseudintermedius infection and colonization in humans is rare. Dog bites are the one circumstance in which there is risk.2 Humans with com-promised immune systems should avoid contact with MRSP-infected dogs.
A recent study demonstrated that MRSP can be present in the home of an MRSP-positive pet.8 Practical hygiene and cleaning are recommended. It is important to wash the pet’s bowl daily and clean any regular sleeping site. Regular washing of collars, leashes, and toys is also recommended. Potentially contaminated bedding, towels, or clothes should be washed separately and dried on a hot setting. MRSP-positive dogs should not sleep on beds with humans.
Because this owner was a nurse, hand hygiene was habitual, but this is not always the case; it may be necessary to specifically state that hand washing should follow contact with the pet or with items with which the pet frequently has contact (eg, food bowls, toys).
The Take-Home
MRSP isolation is increasingly common.
Methicillin resistance means inherent resistance to all β-lactam antibiotics (eg, penicillin, cephalosporin).
MRSP is identified by bacterial culture and susceptibility testing.
Clinical suspicion of MRSP includes lack of treatment response, worsening of signs during treatment, or recurrent infection.
Treatment can be difficult when there is multidrug resistance and no reasonable option for systemic therapy.
Treatment involves concurrent use of systemic and topical antibiotics.
Topical treatment as sole therapy can resolve infections but owner commitment is essential.
Frequent bathing (minimum, 3× weekly) with an antibacterial shampoo (eg, chlorhexidine, benzoyl peroxide, 4% chlorhexidine gluconate with tris-EDTA)
Use of concurrent, topical spot-on therapy (eg, mupirocin)
MRSP has low zoonotic potential, but owners should practice good hand hygiene and wash pet bedding, bowls, and other contact sources.
KAREN A. MORIELLO, DVM, DACVD, is clinical professor of veterinary dermatology at University of Wisconsin–Madison School of Veterinary Medicine. Her clinical research interests include treatment and management of feline dermatophytosis. Dr. Moriello received the 2005 American College of Veterinary Dermatology Award for Excellence for outstanding contributions to service and education and the 2006 Ida Kittleson Award from the Dane County Humane Society for her time and energy contributions in the care of shelter animals with skin disease. Dr. Moriello earned her degree from University of Illinois.