Nerve Blocks for Oral Surgery in Dogs
Brett Beckman, DVM, FAVD, DAVDC, DAAPM, Animal Emergency Center of Sandy Spring, Atlanta, Georgia; Orlando Veterinary Dentistry, Lake Mary, Florida; Florida Veterinary, Dentistry & Oral Surgery, Punta Gorda, Florida

Editor's Note: A previous version of this article incorrectly identified the second maxillary molar in step 2 of Step-by-Step: Caudal Maxillary Nerve Block. It has been corrected as of July 2023.
See the companion article, Nerve Blocks for Oral Surgery in Cats
Nerve blocks are essential before oral surgical procedures are performed in dogs. Not only do nerve blocks provide a basis for pain management in the immediate postoperative period, they also allow for decreased minimum alveolar concentration of inhalant anesthetic, resulting in a safer procedure.
The maximum dose of bupivacaine is determined by patient weight; a safe target maximum dose is 2 mg/kg.1 The volume range of anesthetic infused per site based on patient weight varies (Table).
Table: 0.5% Bupivacaine Infusion Volume per Site Based on Patient Weight
Types of Nerve Blocks
Several types of nerve blocks can be used in oral surgery:
Rostral maxillary (infraorbital) blocks affect bone, teeth, and intraoral soft tissue from the maxillary third premolar rostral to the midline.
Caudal maxillary blocks affect bone, teeth, and intraoral soft tissue from the last molar rostral to the midline, including the ipsilateral soft and hard palatal mucosa and bone.
Rostral mandibular (mental) blocks affect bone, teeth, and intraoral soft tissue from the mandibular second to third premolar rostral to the midline.
Caudal mandibular (inferior alveolar) blocks affect bone, teeth, and intraoral soft tissue from the mandibular third molar rostral to the midline.
Care should always be taken not to inject a vessel. Although rare, resistance when depressing the syringe plunger indicates that the needle may be in the nerve; the needle should be withdrawn and redirected. Extravascular placement can be ensured by aspirating the needle before injection.
Presurgical Considerations
Exact placement of the anesthetic agent is not required. Extravasation of the agent throughout the tissue allows minor deviations in needle placement. However, the more accurate the placement of medication, the less agent required to achieve effect. A canine skull is convenient to have on hand for reviewing anatomic landmarks.
Keeping the patient at a light anesthetic plane can enhance safety and allow the surgeon to confirm effectiveness of the nerve block. If the block was not performed correctly or if the full anesthetic effect has not been achieved, the patient will physiologically react to the initial surgical incision.
Provided the volume of bupivacaine administered is within the maximum recommended volume for the patient’s weight, additional agents can be administered if a particular block is ineffective.
Small- to medium-sized brachycephalic patients do not require a caudal maxillary block. Their short infraorbital canals allow the agent to be placed via the rostral maxillary block to reach nerves before entry into the infraorbital foramen and maxillary bone.
What You Will Need
Syringe (tuberculin to 6 mL, depending on patient size and infusion volume)
Needle (for patients ≤15 kg, 25 gauge, 5/8 inch [0.5 x 16 mm]; for patients >15 kg: 22 gauge, 3/4 inch [0.70 x 19 mm])
0.5% bupivacaine
Optional: canine skull to visualize anatomic landmarks
Step-by-Step: Rostral Maxillary (Infraorbital) Nerve Block
Step 1
To assist with needle placement, visualize the infraorbital foramen that lies dorsal to the distal root of the maxillary third premolar.
Author Insight
Confirm needle placement in the canal before injecting anesthetic. The needle should pass freely into the canal without meeting bony resistance. When correctly placed, the needle will encounter resistance with gentle lateral movement rather than freely moving beneath adjacent alveolar mucosa.

Step 2
Retract the upper lip dorsally to expose the infraorbital neurovascular bundle (arrow) that courses rostral and dorsal from the foramen terminus. This structure can easily be palpated in most canine patients. Advance the needle just rostral to the foramen opening parallel and adjacent to the maxillary bone in a rostral-to-caudal direction. The needle should rest just inside the canal.

Step-by-Step: Caudal Maxillary Nerve Block
Step 1
To assist with needle placement, visualize the ledge of bone just caudal to the second maxillary molar.
Step 2
Insert the needle in a ventral-to-dorsal direction into the soft palatal mucosa where it meets the bone, just caudal to the second maxillary molar. Advance the needle no more than 3–5 mm, depending on patient size, to ensure the tip rests directly under the nerves just before the nerves enter the maxillary bone and infraorbital foramen rostrally.

Step-by-Step: Rostral Mandibular (Mental) Nerve Block
Step 1
To assist with needle placement, visualize the middle mental foramen, which lies just ventral to the distal root of the mandibular second premolar.

Step 2
Retract the mandibular labial frenulum ventrally (arrow). Advance the needle slightly (~15 degrees) ventral and caudal to enter the foramen.

Step-by-Step: Caudal Mandibular (Inferior Alveolar) Nerve Block
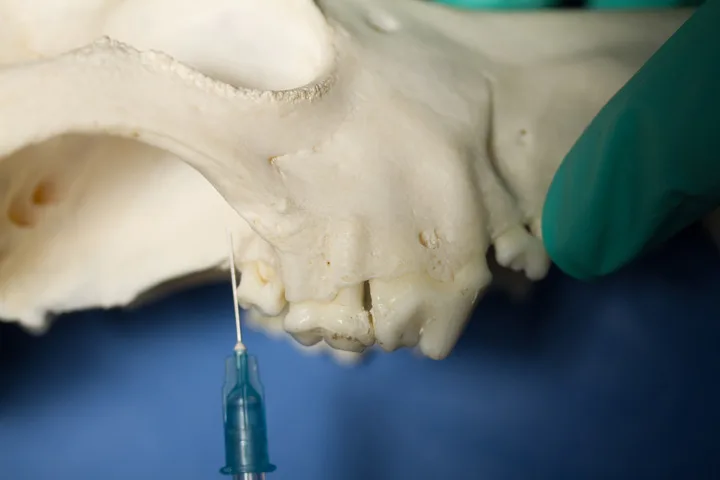
Step 1
To assist with needle placement, visualize the notch in the caudal ventral mandibular body rostral to the angular process. An alternative landmark is the lateral canthus of the eye (Step 2). Dropping an imaginary line directly ventral from the lateral canthus to the ventral mandible allows similar needle placement.
Author Insight
The caudal mandibular block can be administered intraorally; however, it is more technically difficult.

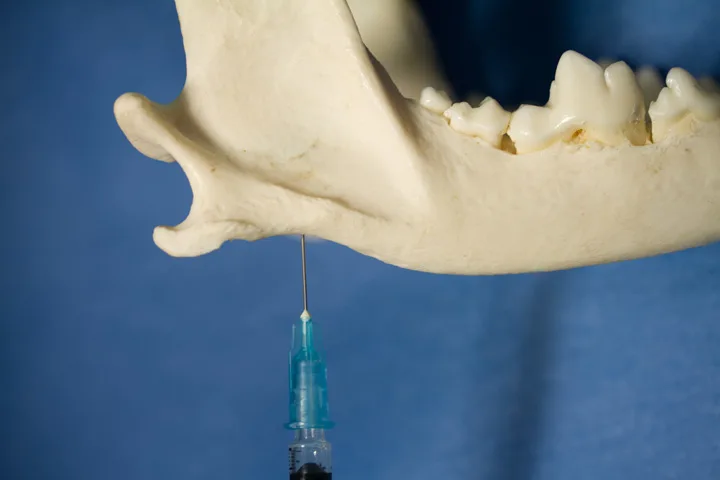
Step 2
Palpate the notch, then direct the needle through the skin toward the lingual aspect of the mandibular body at a 20- to 40-degree angle. Palpation allows tactile confirmation that the tip contacts the bone; the tip should rest just ventral to where the inferior alveolar nerve enters the mandibular canal.
