Multidrug-Resistant Infections
Meike HG Leistra, DVM, Medisch Centrum voor Dieren
Jacqueline Sinke, DVM, Medisch Centrum voor Dieren
The key to successful prevention and treatment of multidrug-resistant (MDR) infections lies in understanding these microorganisms.
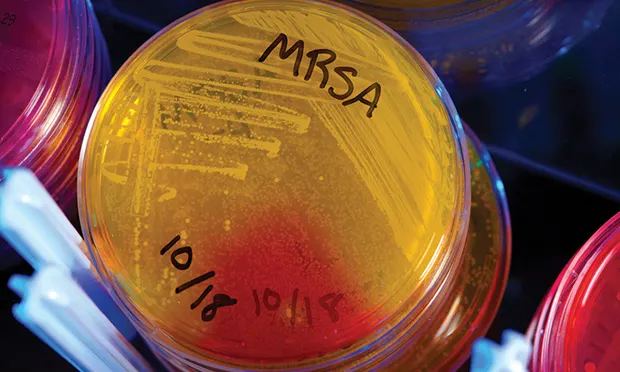
The MDR microorganisms most relevant to companion animal practitioners include methicillin-resistant Staphylococcus aureus (MRSA), methicillin-resistant S pseudintermedius (MRSP), and extended-spectrum b-lactamase–producing Enterobacteriaceae.1 These opportunistic pathogens can cause disease secondary to an underlying medical condition or immune suppression or when normal defensive barriers of the skin or mucous membranes are compromised.2
Related Article: Methicillin-Resistant Staphylococcal Infections
Significance
Routine hygiene before, during, and after contact with patients is the most important measure for preventing infection, particularly in immunocompromised patients and during invasive procedures. Unless the infection’s predisposing factor is identified and treated, recurrence can be expected.
Related Article: Recurrent Pruritus & Zoonotic Potential
Figure 1. Pyoderma caused by a multidrug-resistant infection.

MDR infections do not cause specific diseases, but because of their colonization preferences, the following presentations in companion animals are frequently associated with these microorganisms3-6: pyoderma (Figure 1), otitis externa, nonhealing wounds, implant infections, and urinary tract infections. In these infections, diagnostic investigation, preferably by bacterial culture and susceptibility testing, is strongly advised.
The clinical nature of an infectious disease does not indicate anything about susceptibility of the pathogen.7 Infection caused by an MDR microorganism distinguishes itself clinically from an infection caused by a susceptible microorganism based on the lack of response to appropriate antimicrobial therapy. An MDR infection should be suspected when an infectious disease does not respond to the appropriate antibiotic. Bacterial culture and susceptibility testing should be performed in these cases.
Routine Strategies for Reducing Risk
Every veterinary practice should have a protocol that describes strategies for reducing infection risk. The protocol can be adapted from various available guidelines8,9 to meet the specific requirements of each practice. Protocols for hand hygiene (see Hand Hygiene), use of personal protective equipment, cleanliness and disinfection of environment, laundry, and waste management should be addressed.
Recurrent Skin Infection: Treatment & Owner Education
| Because hands are the primary vehicle for pathogen transmission in any healthcare setting, hand hygiene is essential for infection prevention. The goal is to reduce the number of microorganisms present, not to sterilize the hands. Skin irritation should be prevented, as it increases survival and growth of bacteria.
Hand hygiene can be maintained by using an alcohol-based hand sanitizer or by regular hand washing. An alcohol-based hand sanitizer is the preferred method because of its effectiveness in reducing contamination; this method is also less detrimental to the skin than repeated soap use.12,13,16 Soap is only necessary after bathroom use or when the hands are visibly dirty or soiled.
Hand hygiene should be performed:
Before and after patient contact
Before aseptic and/or invasive procedures
After possible contamination of the hands with body fluids or after contact with mucous membranes or open wounds
When moving from a contaminated body site to another body site during care of the same patient
After removing gloves
|
Judicious Use of Antimicrobial Drugs
Prudent use of antimicrobials is a powerful tool in preventing the uninhibited spread of MDR microorganisms in veterinary medicine.10 This involves using antimicrobials only when needed, such as when pathogenic bacteria are likely involved in the disease process and, if possible, confirmed by diagnostic procedures.11,14
Ideally, antibiotic choice should be based on bacterial culture and susceptibility testing. When choosing an empiric antibiotic, it is important to note that narrow-spectrum antibiotics are no less potent or useful than other drugs.
Antimicrobial agents that are critical to animal and human health should not be used without bacterial culture and susceptibility testing (see Global Relevance). The affected organ systems, site of infection, most likely causal pathogen, and pharmacokinetic properties of the drug should also be considered.11,14
The optimal dose should always be used for the necessary length of time. Response to treatment should be measured and the dosage and drug choice adjusted as needed.
How I Treat: MDR Infections
Treat the patient14,15
Identify and treat or control the underlying disease.
Select therapies that do not involve antimicrobials when possible (eg, proper wound management and debridement, topical antiseptic therapy).16,17
Select antibiotics based on bacterial culture and susceptibility testing.
Do not use antibiotics that are critically important to human health.
These are defined by the World Health Organization (WHO) as antibiotics that are the sole therapy or one of the few alternatives for the treatment of serious human diseases and antibiotics that are used to treat diseases caused by zoonotic organisms or organisms that may acquire resistance genes from nonhuman sources.
Cephalosporins (third and fourth generation), macrolides, and quinolones are classified as the antimicrobials most critical for human medicine by WHO, Food and Agriculture Organization of the United Nations, and World Organisation for Animal Health (see Global Relevance).
Monitor the effectiveness of therapy regularly through bacterial culture and susceptibility testing.
Keep the clinic free of MDR infection18
When patients with known or suspected MDR infection come to the clinic, minimize contact with other patients, especially surgical or immunocompromised patients.
Ideally, use an isolated examination room with a separate entrance and waiting area.
Alternatively, schedule the appointment for the end of the day and limit the number of rooms the patient visits.
Clean and disinfect rooms that have been used by an MDR patient using a standard protocol before another patient is allowed to enter.
Do not hospitalize MDR patients unless an isolation area is available.
Protect the veterinary team18
Team members handling patients with known or suspected MDR infection should take additional personal protection measures to reduce the risk for direct transmission to other animals and humans and to minimize fomites.
Use gloves and single-use protective outerwear (ie, gown or laboratory coat that is discarded or laundered after use).
Communicate with clients
Educate the owner about the animal and human health risks associated with MDR infections.
Provide the client with instructions about hygienic conduct concerning contact with the patient, materials about zoonotic diseases, and information about prevention (eg, hand washing, child supervision, glove use).
Provide information sheets and/or a reliable website address for more information.
| The problem of antimicrobial resistance is internationally widespread. A concerted effort among nations and the adoption of policies of prudent antimicrobial use are needed.
In some countries, specific guidelines for prudent use of antimicrobials in companion animals have already been developed. The exact guidelines may differ depending on the local situation and must be updated regularly. Also, regulations concerning the use of certain human antibiotics not licensed for animals may differ among countries.
The most up-to-date and relevant information regarding appropriate drug selection is likely to be published by national veterinary organizations.19-21
Nicole Rego, BVSc, MVScMumbai, India
|
MDR = multidrug resistant, MRSA = methicillin-resistant Staphylococcus aureus, MRSP = methicillin-resistant Staphylococcus pseudintermedius