Multidrug-Resistant Enterococcal Infections
You have asked…
I have isolated a multidrug-resistant Enterococcus species. What’s next?
The expert says…
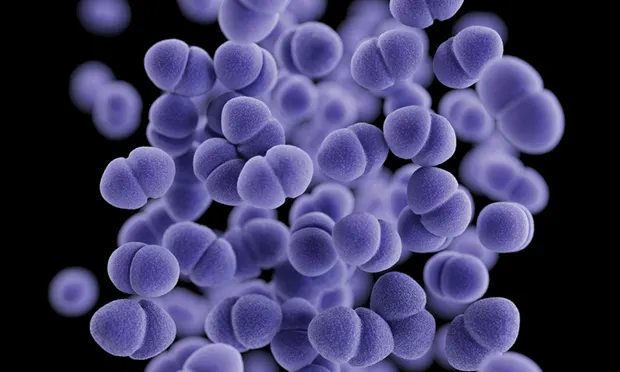
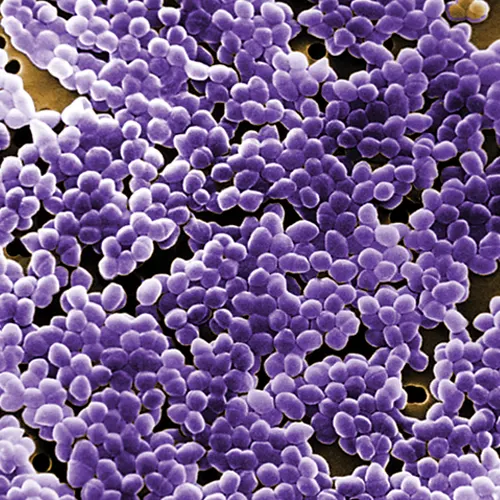
Enterococci are gram-positive bacteria that are widely found in all types of animals and in the environment. They are ubiquitous members of the commensal microbiota and are typically harmless inhabitants of various body sites—particularly the intestinal tract. However, enterococci are opportunistic pathogens that can cause a wide range of signs if the circumstances are advantageous.
Although enterococci are relatively easy to isolate, determination of clinical relevance may be a challenge. In addition, enterococci are inherently resistant to many antimicrobials, including penicillin, clindamycin, trimethoprim–sulfamethoxazole, and low levels of aminoglycosides, and they are poorly responsive to cephalosporins and fluoroquinolones in vivo.
Although enterococci are relatively easy to isolate, determination of clinical relevance may be a challenge.
Enterococci may also acquire resistance to many other antimicrobials, resulting in multidrug-resistant strains with limited treatment options. For example, vancomycin-resistant enterococci (VRE) are of particular concern in human healthcare. VRE can be isolated from companion animals,1,2 but clinically relevant infections are rarely reported. However, even vancomycin-susceptible enterococci may be resistant to a wide range of antimicrobials, leaving few viable treatment options in some cases.
When addressing with a potential enterococcal infection, a few questions should be considered.
Related Article: Multidrug-Resistant Infections
Is this Enterococcus species relevant?
Determining whether treatment is needed for an infection with an Enterococcus species is an important first step, but the answer is not always clear. Enterococci are common inhabitants of different body sites and have relatively limited virulence. It is impossible to give absolute guidance, but general considerations are presented in Table 1.
The two main pathogenic enterococcal spp are E faecium and E faecalis. A variety of other species can be encountered, but the clinical relevance of those species is variable. Some have been associated with disease in humans or animals (eg, E casseliflavus, E avium, E durans, E gallinarum) but not all enterococci are recognized as being clinically important. Enterococci other than E faecium and E faecalis should not be dismissed, but additional thought should be given to their clinical relevance when they are isolated.
It is important to remember the degree of antimicrobial resistance has no impact on the decision to treat. Highly resistant isolates are no more inherently virulent than susceptible isolates. If a susceptible Enterococcus spp would be considered clinically irrelevant, the same would apply to a multidrug-resistant isolate from the same sample.
What are the available antimicrobial options?
Results of culture and susceptibility testing will guide treatment. Clinical and Laboratory Standards Institute (CLSI) guidelines dictate that laboratories should not report susceptibility results for drugs to which enterococci are inherently resistant or where there is poor efficacy in vivo (ie, penicillin, clindamycin, trimethoprim-sulfamethoxazole, cephalosporins, low-level aminoglycosides),3 so susceptibility panels may contain few drugs.
Related Article: Antibiotics in Surgical Patients
Ampicillin or amoxicillin are the drugs of choice in isolates susceptible to these drugs. While enterococci have inherent low-level aminoglycoside resistance, aminoglycosides may be useful in combination with amoxicillin or ampicillin when isolates do not demonstrate high-level aminoglycoside resistance. Combination therapy can be effective because bacterial cell wall damage from ampicillin or amoxicillin facilitates entrance of the aminoglycoside into the cell, even if the isolate is resistant to ampicillin/amoxicillin and gentamicin individually.
Many laboratories report whether the isolate is susceptible to high-level gentamicin (or gentamicin/ampicillin synergy), and this combination is a good option when amoxicillin or ampicillin resistance is reported and when other options are limited.
CLSI guidelines dictate that laboratories should not report susceptibility results for drugs to which enterococci are inherently resistant or where there is poor efficacy in vivo ... so susceptibility panels may contain few drugs.
Fluoroquinolones tend to work poorly for systemic enterococcal infections and are typically not recommended for infections other than those in the urinary tract. Recently, breakpoints for ciprofloxacin and levofloxacin for the treatment of urinary tract infections in humans were proposed,4 and this drug class may be useful in animals. However, efficacy data are lacking. E faecium—but not E faecalis—is also inherently resistant to carbapenems, which further reduces treatment options.
Chloramphenicol may be useful in some situations, such as when the isolate is susceptible in vitro. Patient and owner safety must be addressed when considering this drug, which can be an effective option in situations where other drugs are limited and owners can properly handle the drug. Additional options may be available for urinary tract infections, such as nitrofurantoin and fosfomycin.
In rare cases, isolates may be resistant to all commonly used drugs and susceptible only to drugs such as vancomycin or linezolid. There are ethical debates about the use of these types of drugs in animals because of the need to balance public health with animal health and welfare. These drugs should be rarely needed and rarely used, and careful consideration should be made before using them (see Checklist for Use of Vancomycin or Linezolid).
The public health implications of rare and appropriate use of these drugs are likely inconsequential, but some potential for resistance exists with any use of an antimicrobial, so the concerns should not be dismissed.
Use of these drugs is prohibited in some countries. In addition, some veterinary facilities voluntarily prohibit use of these drugs or restrict their use to situations where a detailed set of criteria have been fulfilled—typically with approval by an infectious disease expert.
How do I manage this resistant infection?
The general approach to treatment of a resistant enterococcal infection is no different than treating an infection caused by a susceptible isolate. Resistant pathogens can be associated with worse outcomes, but that is typically because of the failure of empiric antimicrobial therapy. After the cause is known and an appropriate antimicrobial has been identified (if a viable antimicrobial option can be found), there should be no difference in prognosis and management for resistant versus susceptible pathogens.
While resistant strains may need different antimicrobials, resistance should not impact other aspects, such as duration of treatment and whether other measures (eg, surgery) are required.
Additional considerations
Enterococci are important hospital-associated pathogens in humans,5,6 and they can cause significant problems in healthcare facilities because of susceptible populations.
Enterococci are also able to persist in the environment better than some other pathogens7 and can commonly be found in veterinary hospitals,8,9 although they are readily inactivated by proper disinfection.
Enterococci are transmitted by direct and indirect contact, not airborne or aerosol routes, so proper use of standard practices (ie, personal protective equipment, hand hygiene, environmental cleaning and disinfection) should minimize risk of transmission.
Although objective data are lacking, it is reasonable to use enhanced infection control practices for animals with multidrug-resistant enterococcal infections when they are in the clinic. This would include physical separation (isolation or using other housing and handling practices) and use of personal protective equipment, hand hygiene, cleaning, and disinfection to minimize the risk for direct or indirect exposure.
There are limited concerns about zoonotic transmission of enterococci. While clear evidence of human–animal transmission is lacking, molecular studies have identified the same types of enterococci in humans and animals,2,10 suggesting that there may be some risk. However, enterococci are shed by virtually all animals (meaning human exposure would be high), so the risk must be low considering the lack of convincing evidence that animals are a relevant source of human infection.
The potential for zoonotic infection should not be dismissed, particularly for humans at increased risk for infection (eg, the young, the elderly, pregnant women, immunocompromised persons) are present, but routine infection control and hygiene practices should minimize any risk.
VRE = vancomycin-resistant enterococci
J. SCOTT WEESE, DVM, DVSc, DACVIM, is veterinary internist and microbiologist, chief of infection control at University of Guelph, Ontario Veterinary College Health Sciences Centre, and Canada Research Chair in zoonotic diseases. Dr. Weese’s research foci are infectious and zoonotic diseases (particularly of companion animals), infection control, staphylococcal infections, Clostridium difficile infection, and antimicrobial therapy. After earning his DVM and spending time in private practice, he completed a large animal internal medicine residency and Doctor of Veterinary Science graduate program. He is board certified in internal medicine by the American College of Veterinary Internal Medicine and is chief of infection control at Ontario Veterinary College Teaching Hospital.