Liver Ultrasound-Guided Fine-Needle Aspiration
Daniel VanderHart, DVM, DACVR
Clifford R. Berry, DVM, DACVR, University of Florida
Although ultrasonography of the liver can be sensitive for detecting hepatic disease, actual sonographic changes are often nonspecific.1-3
Ultrasonographic changes (eg, diffusely increased/decreased hepatic echogenicity, heterogeneity) are considered indications for sampling (Figure 1). The sonographer needs to be skilled to ensure image optimization for accurate interpretation of hepatic echogenicity; operator error (eg, increasing/decreasing the gain setting) can impact organ echogenicity and interpretation (see Required Sonographic Skills for Fine-Needle Aspiration). Evaluation for multicentric lymphoma or mast cell disease is also an indication for general liver sampling, even in patients without ultrasonographically detectable abnormalities (Figure 2).4-6

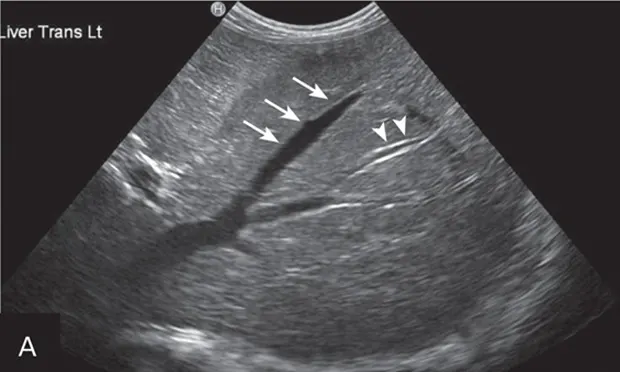
Figure 1A
In each of these cases, histologic diagnosis was made using fine-needle aspirates of the liver (vacuolar hepatopathy, hepatic lipidosis, acute severe neutrophilic hepatitis, respectively). Transverse image (A) of the left side of the liver in a normal dog showing hepatic vein (arrows) and portal vein (arrowheads). Hyperechoic liver (B) secondary to glycogen accumulation resulting from Cushing’s disease in a dog. Note the decrease in portal vascular markings. Hyperechoic and hyperattenuating liver (C) secondary to hepatic lipidosis in a cat. Note the hypoechoic falciform fat in the near field (≤1.5 cm deep) relative to liver echogenicity. In addition, there are some contact artifacts resulting in hyperechoic lines as well as the normal lines of abdominal musculature in the extreme near field (<0.5 cm). In normal cats, falciform fat and hepatic echogenicity are isoechoic to each other. In the far field, hyperattenuation of the ultrasound beam results in image dropout (starting at a depth of 3.5 cm). Hypoechoic liver (D) secondary to acute hepatitis in a dog. Note the marked decrease in echogenicity relative to the spleen.

Figure 2A
Liver with normal parenchymal echogenicity in a dog (A); however, cytologic examination via fine-needle aspirate showed diffuse infiltration of malignant mast cells. Liver with normal ultrasonographic appearance in a cat (B); however, cytologic examination via fine-needle aspirate showed diffuse infiltration with lymphoblasts indicative of lymphoma.
Sample evaluation of focal lesions is often recommended as these lesions can have multiple sonographic appearances: anechoic, hypoechoic, hyperechoic, or mixed echogenicity (Figure 3). Specific differentials for focal hepatic lesions should not be determined solely on ultrasound abnormalities, given the sonographic variation.1 Cytology should be considered a screening tool because its agreement with histopathologic diagnosis of various liver diseases is reportedly 30.3% in dogs and 51.2% in cats.7 Inflammatory hepatic diseases were diagnosed in only 5 of 20 dogs and 3 of 11 cats in one study7; cases of hepatitis may be missed on cytology.

Figure 3A
Focal hepatic lesions demonstrating multiple appearances on ultrasound: Hypoechoic nodule representing nodular regeneration in a dog (A). Hyperechoic nodule representing metastatic carcinoma in a dog (B). Cavitated hyperechoic nodule representing benign cystadenoma in a cat (C). Mixed-echogenic nodule with target-like appearance representing metastatic sarcoma in a dog (D). Mixed-echogenic, cavitated hepatic mass representing hepatocellular carcinoma in a dog (E).Large hypoechoic mass representing histiocytic sarcoma in a dog (F). Two anechoic nodules representing benign hepatic cysts in a dog (G).
Required Sonographic Skills for Fine-Needle Aspiration
Fine-needle aspiration should only be attempted by skilled sonographers who can:
Efficiently operate the ultrasound machine
Consistently produce high-quality images
Optimize the images for near field structures
If the target or lesion is >1.5 inches from the skin surface, the sonographer will be unable to obtain the aspirate because of artifacts related to propagation speed errors and larger, centrally located vascular structures.
Understand the physics behind propagation speed errors, particularly in obese patients
This is essential to prevent the sonographer from placing the needle deeper in the tissues than it appears on the image.
Fine-tune the image with the ultrasound probe using nondistance rotational and oblique motions
Routinely perform ultrasound-guided cystocentesis