Limb Swelling in an Intact Boerboel
Michael Hung, DVM, Texas A&M University
Carly Patterson, DVM, DACVIM (SAIM), Texas A&M University

Clinical History & Signalment
Hercules, a 200.6-lb (91-kg), 15-month-old intact male Boerboel, was presented to a referral clinic for a swollen left hock of 5 months’ duration. Swelling was seen after Hercules had been boarded. He was purchased from a breeder in Illinois at 9 months of age and lived in northeast Texas. He was otherwise healthy.
An immunosuppressive dosage of prednisone (40 mg/m2 PO every 24 hours, tapered over 15 days) and amoxicillin/clavulanic acid (9.9 mg/kg PO every 12 hours for 10 days) were administered. Carprofen (2.2 mg/kg PO every 12 hours for 14 days) was given after prednisone had been tapered with a 72-hour washout period. No improvement was seen. Radiographs of the affected leg taken by the referring clinician were unremarkable.
Physical Examination
On physical examination at the referral clinic, Hercules was bright, alert, and responsive. Initial temperature was elevated (103.2°F [39.6°C]), but recheck temperature was normal (101.4°F [38.5°C]). He was weight-bearing on all limbs. The left pes and tarsus were diffusely swollen with nonpitting edema (Figure 1). The dorsal tarsus was thickened, and the third digit was swollen circumferentially with severe erythema and crusting at the level of the claw (Figure 2). No warmth was appreciated. Hercules appeared to mildly resist manipulation of the toe but did not seem otherwise painful. The left popliteal lymph node was mildly enlarged and firm. Diffuse scaling was present over the tail base, and crusting papules and collarettes were distributed asymmetrically over the trunk, tail base, and extremities. The remainder of the physical examination was unremarkable.

Edematous appearance of the left tarsus and swollen third digit, especially compared with the contralateral limb

Enlargement, erythema, and crusting at the distal aspect of the third digit at the level of the claw
Diagnosis
Differential diagnoses for a single swollen limb include increased hydrostatic pressure from arteriovenous fistula or obstruction caused by trauma, foreign body, or neoplasia; increased capillary permeability from envenomation, trauma (including foreign body), burn, or infectious cellulitis; and lymphatic drainage dysfunction from lymphangiosarcoma or lymphedema (see Take-Home Messages).
CBC showed a mature neutrophilia (17,864/µL; reference interval, 3,000-11,500/µL), and serum chemistry profile revealed mildly increased globulin (4.2 g/dL; reference interval, 1.7-3.8 g/dL).
Radiographs of the left pelvic limb revealed soft tissue swelling of the digit and tarsus with no bony involvement, and cytology of the left popliteal lymph node showed reactive lymphoid hyperplasia. Fundic examination results and thoracic radiographs were unremarkable.
The affected digit was clipped, cleaned, and examined with the patient under sedation; ulcerated wounds were present, but no draining tract was noted (Figure 3). Cytology was not performed due to high likelihood of contamination because of the location of the wound and because bacteria in the region were likely significantly reduced during preparation. Surgical biopsies with the patient under general anesthesia were planned.

Ulcerated lesions on the digit after hair was clipped
Hercules was anesthetized for lymphangiogram, surgical biopsies of the dorsal tarsal and digital skin and subcutaneous tissues, and pelvic limb CT (to assess for subtle bony lesions and vascular malformation). Lymphangiogram was normal. Tissue from the digit was submitted for aerobic and anaerobic culture for Nocardia spp and Actinomyces spp growth; one colony of Staphylococcus epidermidis (likely a contaminant) was present. Histopathology of the digit showed severe, regionally extensive, chronic pyogranulomatous panniculitis with rare intralesional yeast most consistent with Blastomyces spp (Figure 4). Mild, diffuse, chronic perivascular lymphoplasmacytic panniculitis of the dorsal tarsus was also noted, likely secondary to Blastomyces spp infection.
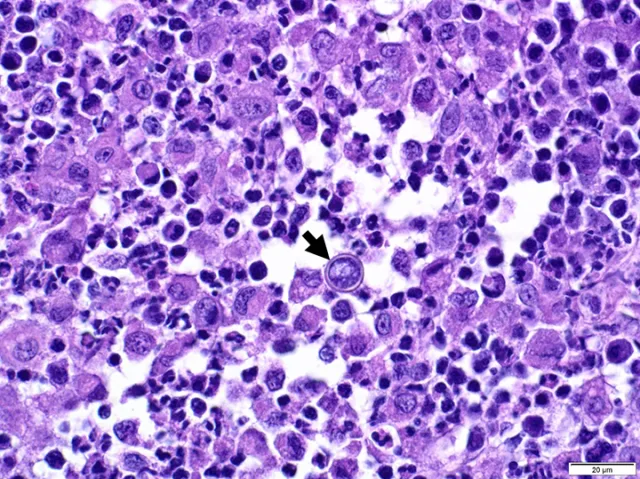
Histopathology showing multifocal-coalescing pyogranulomatous dermatitis and panniculitis and intralesional fungal yeast (arrow). Hematoxylin and eosin stain, 60× magnification. Image courtesy of Dominique Wiener, Dr.med.vet, PhD, DECVP
CT showed soft tissue thickening of the third digit and distal portion of the left limb consistent with edema or cellulitis and left popliteal lymphadenomegaly with no evidence of a mass, foreign body, or vascular malformation.
Urine quantitative antigen test result was positive for Blastomyces spp (0.48 ng/mL; quantifiable range, 0.2-14.7 ng/mL).
Illinois is an endemic state for blastomycosis. Hercules was likely infected via inoculation (based on localized signs) while still with the breeder, and development of clinical signs after boarding was likely incidental. Stress may have resulted in immunocompromise that contributed to infection.
Cutaneous lesions (ie, collarettes, pustules) on the trunk, tail base, and extremities were consistent with presumed clinical bacterial pyoderma.1,2
Diagnosis: Blastomycosis
TREATMENT AT A GLANCE
Oral itraconazole is the first-line treatment for blastomycosis.
Fluconazole can have similar efficacy as and is less expensive compared with itraconazole; however, longer treatment periods may be needed.
Liver enzymes should be evaluated monthly with azole treatment. Clinically affected areas should be checked monthly to monitor progression or regression of disease.
Serial urine antigen tests can be performed every 3 months and can indicate successful treatment. A decrease in antigen concentration is consistent with effective treatment.
Fungal infections require prolonged treatment over months. Relapse may occur, even with appropriate treatment.
Treatment & Management
Fluconazole (11 mg/kg PO every 24 hours) was administered based on the patient’s large weight (due to cost) and because severe systemic disease was not present (see Treatment at a Glance). Collarettes and scaling were considered secondary to presumptive superficial bacterial pyoderma and treated topically with chlorhexidine gluconate 2%/miconazole nitrate 2%/tris-EDTA shampoo.
Blastomycosis can exhibit testicular tissue tropism.3 Neuter was recommended, especially due to possible relapse, but the owner declined.
Prognosis & Outcome
At the one-month recheck, neutrophilia (12,000/µL; reference interval, 3,000-11,500/µL) and hyperglobulinemia (4 g/dL; reference interval, 1.7-3.8 g/dL) were improved, the digit was no longer ulcerated, and swelling and erythema had improved; however, the digit and hock were still enlarged (Figure 5). Treatment was continued.

Improved appearance of dermatologic lesions on the digit after one month of treatment with fluconazole
At the 2-month recheck, the owner reported Hercules was doing well, but the digit and foot remained swollen (Figure 6). ALT was elevated (258 U/L; reference interval, 10-125 U/L), which was attributed to liver enzyme activation due to fluconazole therapy, and the dose was reduced by 40%. A 3-month recheck was recommended to evaluate antigen concentrations, but the patient was not returned.
Hercules’ overall prognosis was positive, but prognosis for return to a normal digit and tarsus was guarded.

Affected tarsus after 2 months of treatment. Erythema and swelling had improved, but the digit and tarsus remained enlarged.
Discussion
Blastomycosis is a systemic disease caused by Blastomyces dermatitidis, a broad-based dimorphic fungus found in the soil around the Ohio and Mississippi River valleys, the Great Lakes, and southeastern states; the primary route of infection is the respiratory tract. Common sites of disseminated infection include the skin, subcutaneous tissue, eyes, bones, lymph nodes, brain, and testes.1,2
Dermatologic signs can be seen with blastomycosis; 30% to 50% of dogs have cutaneous signs at diagnosis.1,4 Incidence of dogs presented solely for localized cutaneous signs is not well described, although one study noted only 13% of dogs with blastomycosis had no radiographic pulmonary changes.4 Thoracic radiographs were unremarkable in this case.
Diagnosis is made by identifying the organism via cytology, histopathology, culture, or antigen testing.5 Histoplasmosis should be ruled out in patients that live in states where both Histoplasma spp and Blastomyces spp are endemic, as Histoplasma spp can cross-react with Blastomyces spp quantitative antigen testing on both urine and serum.5 Cytology of the affected digit in this case could have resulted in diagnosis, but more extensive sampling under anesthesia was preferred.
Definitive diagnosis involves respiratory sampling, which is not often pursued without other evidence of involvement. In humans, primary cutaneous blastomycosis is rare, and differentiation from secondary cutaneous blastomycosis with negative thoracic radiography is difficult.6,7
Itraconazole is the treatment of choice for blastomycosis, but amphotericin B can be administered parenterally in dogs with severe disease or CNS disease or in dogs refractory to treatment.1,8 Fluconazole can also be used but is considered less effective than itraconazole for non-CNS disease in humans.8-10 One study found similar efficacy in dogs administered fluconazole or itraconazole; fluconazole treatment had longer duration but was less expensive.11
Treatment generally lasts ≥3 months and should be continued 1 month beyond resolution of clinical signs. Radiography should be performed at 4- to 6-week intervals if abnormalities are present on thoracic imaging. Liver enzymes should be monitored with any azole treatment (generally at 2 weeks, then at 4- to 6-week intervals). Urine antigen tests can help monitor disease progression and can be performed every 3 months; antigen reduction is associated with appropriate treatment. Remission can be determined by normal physical examination and normal or static imaging (eg, thoracic radiographs) findings.12 Approximately 50% to 75% of dogs with blastomycosis respond to treatment, but 20% can relapse, usually within one year.12-14
One study found dogs with absent or mild pulmonary radiographic signs and low Blastomyces spp antigen concentrations survived ≥1 year after diagnosis.15 Chronic inflammation, persistent edema, and panniculitis can result in fibrosis, similar to chronic lymphedema.16,17 Persistent swelling may indicate persistence of disease, as most fungal infections require treatment for >2 months.1,12,15
TAKE-HOME MESSAGES
A problem-based approach with attention to anatomy (including vascular and lymphatic causes) and localization of signs should be used in patients with limb swelling.
Advanced imaging may be needed to rule out lymph node obstruction and vascular malformation.
Thorough examination for infectious etiologies, including histopathology and tissue culture, should be performed in patients with limb swelling.
Blastomycosis is a disseminated disease in dogs; localized infections are possible. Most patients are presented with predominantly respiratory and/or cutaneous signs.
Histoplasmosis should be ruled out in patients with a positive Blastomyces spp quantitative antigen test result, and blastomycosis should be ruled out in patients with a positive Histoplasma spp quantitative antigen test result in regions endemic to both of these fungi.