Emergency Urinary Bladder Surgery
Grayson Cole, DVM, University of Tennessee
Karen M. Tobias, DVM, MS, DACVS, University of Tennessee
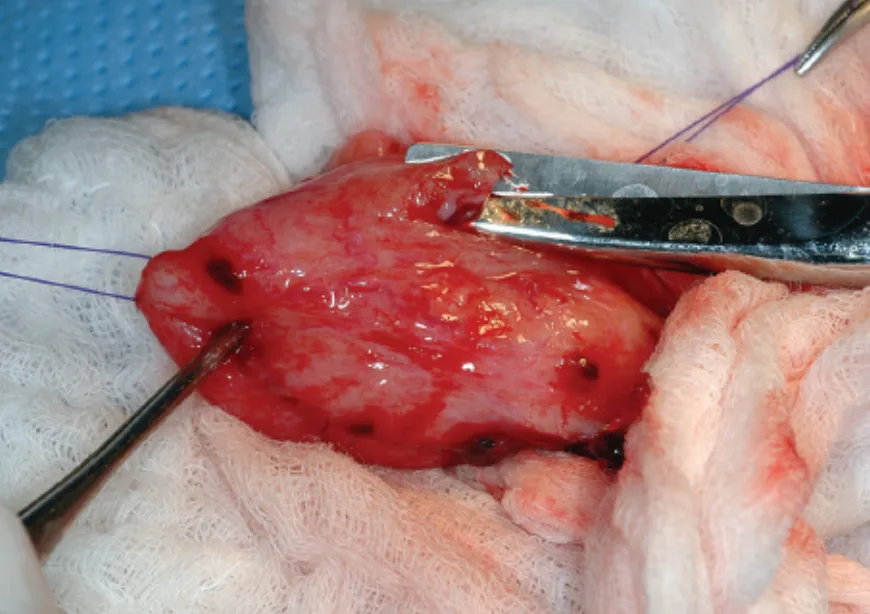
Urinary bladder surgery in small animals is typically performed as an elective procedure, usually to remove calculi; however, certain conditions (eg, urethral obstruction or urinary bladder entrapment, torsion, rupture) may warrant immediate intervention. When possible, patients should be managed with urinary diversion until they are hemodynamically stable. Immediate surgery is indicated when bladder necrosis is a concern (eg, bladder herniation, torsion) or attempts at urinary diversion fail (Figure 1).

Blunt abdominal trauma resulted in herniation of the bladder through a rectal tear in this Jack Russell terrier (1.5 years of age). Bilateral ureteral avulsion was confirmed during exploratory surgery.
Preoperative Management
Patients with uroabdomen or urinary tract obstruction frequently present with electrolyte and metabolic derangements, dehydration, and hypotension. Hypotension and hyperkalemia can be life threatening and should be addressed immediately. Patients should be fluid resuscitated with an isotonic crystalloid solution. Historically, 0.9% saline was recommended because of its lack of potassium; however, lactated Ringer’s solution may be as effective as 0.9% saline in reducing potassium concentrations and more efficient in normalizing acid-base status and other electrolytes.1
Hyperkalemia can usually be corrected with fluid administration and resolution of urine retention; however, specific treatment (Table) is indicated with hyperkalemia-induced ECG abnormalities (eg, bradycardia, absent P waves, widened QRS complexes, tented T waves).
Table: Treatment of Hyperkalemia
Resolution of urine retention is critical for normalizing electrolytes and acid-base status and resolving azotemia. Urinary diversion can be performed with an indwelling urethral catheter, intermittent cystocentesis, peritoneal drainage, or percutaneous cystostomy tube placement.
Although controversial, cystocentesis can be used for short-term bladder decompression. Use of cystocentesis, analgesics, sedation, and SC fluids was reportedly successful for nonsurgical resolution of urethral obstruction in 11 of 15 cats.2 Ultrasonographic guidance during cystocentesis may help confirm that the bladder has completely emptied.
If the urinary tract has ruptured, urinary diversion may be accomplished by inserting a peritoneal drainage catheter, Jackson-Pratt drain, or multifenestrated chest tube aseptically with the patient under local anesthetic and sedation.
Severe azotemia can be treated by peritoneal dialysis. Commercial dialysates are available; however, lactated Ringer’s solution with 1.5% dextrose (30 mL 50% dextrose added to 1-L bag) can be used for short-term treatment of a normovolemic patient. Warmed dialysate solution can be infused at a rate of 10 to 20 mL/kg over 10 to 15 minutes, allowed to sit in the peritoneal cavity for 45 minutes, then drained. Dialysis may be repeated q4h until definitive treatment or long-term urinary diversion can be accomplished. Complications include hypoalbuminemia, peritonitis, catheter failure, and electrolyte imbalances.
Cystostomy tubes can accommodate longer-term urinary diversion. Percutaneous cystostomy tube placement under fluoroscopic guidance (which may also permit antegrade urethral catheterization to resolve obstruction) has been described but used infrequently; it requires advanced imaging and technical skills and may take as long as or longer than some surgeries. Cystostomy tubes and urinary and abdominal catheters should be connected to a closed collection system to help lower risk for ascending infection.
Related Article: The Case: Remnant Urethral Calculus After Cystotomy
Related Article: Urinary Obstruction: Treatment Measures
Expert Tips
Use a needle and syringe connected to a 3-way stopcock for cystocentesis and to empty the bladder fully. Once the bladder is empty, its wall contracts and thickens, sealing the puncture.
Almost all types of peritoneal catheters quickly obstruct with omentum and usually lose functionality within 24–72 hours.
Once repaired, full-thickness defects of the urinary bladder can regain 100% of normal tissue strength in 21 days.
Perioperative Management
Because animals usually require intraoperative urethral catheterization, the perineum and prepuce or vulva should be included in the surgical preparation. The prepuce should be flushed with dilute chlorhexidine (0.05%) solution to reduce bacterial content. A purse-string suture can be placed in the anus to prevent intraoperative fecal leakage. Bladders entrapped in hernias should be decompressed with a urinary catheter or by cystocentesis.
The bladder is usually approached through a ventral midline incision of the abdominal musculature. In male dogs, skin and SC incisions curve around the prepuce, requiring ligation of the external pudendal vessels. The bladder should be incised on the ventral or apical surface, when feasible, to reduce risk for iatrogenic damage to ureters. Cystectomy may be required because of necrosis or neoplasia; in dogs, approximately 70% of the bladder may be removed without significant consequence.
The neurovascular supply to the bladder enters via the trigone region, which is also the site of regenerating epithelium; it is thus important to leave the trigone area intact.
In the described case (see Step-by-Step), perineal urethrostomy and cystotomy were performed concurrently while the patient was in dorsal recumbency to remove uroliths and permit concurrent correction of a urethral stricture.
Cystotomy closure can be performed with fine-gauge (3-0 to 5-0) monofilament, rapidly absorbable suture. Single-layer continuous appositional suture patterns are as effective as two-layer inverting patterns and faster to perform. Interrupted patterns can be used if the closure is irregularly shaped, as with partial cystectomy. Bites should include submucosa; full-thickness bites should be avoided because of risk for calculus formation. If the blood supply is questionable, omentum can be wrapped around the bladder and tacked with interrupted, absorbable sutures. Serosal patches have also been used to improve blood supply, but omentum may work better.
If neoplasia is suspected, new surgical gloves and instruments should be used after the mass has been removed. If a perineal hernia is present, cystopexy and colopexy can be performed before abdominal closure.
Related Article: Feline Urolithiasis
Postoperative Management
Indications for placement of an indwelling urinary catheter and/or cystostomy tube after bladder surgery include extensive partial cystectomy, urethral damage, persistent obstruction, or evidence of bladder atony. A cystostomy tube may be more appropriate if prolonged urinary diversion is expected.
Indwelling urinary catheters should remain in place for the shortest duration possible, as risks for urinary tract infection (UTI) can increase by 20% each day the catheter is in place. Because systemic antibiotics may increase risk for UTI, they are not routine during catheterization (except for preexisting infection).1 After the urinary catheter has been removed, urine culture can determine the need for antibiotic therapy.
Postoperative analgesia is typically accomplished with opioids. NSAIDs provide analgesia and may decrease bladder inflammation but should be withheld until patients are normovolemic and hydrated.
Potential complications of cystotomy include abdominal incision issues, dehiscence of the cystotomy closure (rare), and incomplete removal of uroliths. Presence of residual calculi may be noted in up to 14% of dogs and 20% of cats after cystotomy; therefore, postoperative imaging is recommended to ensure all calculi have been removed. Calculi should be analyzed if the composition is unknown.
Step-by-Step: Cystotomy
What You Will Need
Laparotomy sponges
18-gauge needle and sterile syringe (to empty bladder)
3-0 monofilament suture material on a tapered needle (for stay sutures)
Scalpel (#10 or #15)
Metzenbaum scissors
Hemostats (for stay sutures)
Bladder spoon (if calculi are expected)
Rigid scope with retrieval basket
Suture scissors
Debakey thumb forceps
Sterile saline and a large sterile or bulb syringe
Transurethral urinary catheter or cystostomy tube
3- to 10-French red rubber catheter (for female dogs)
Foley (female dogs) or retrograde catheter
Needle holders
Busse Poole suction tip
3-0, 4-0, or 5-0 rapidly absorbable, synthetic monofilament on a taper needle (for bladder closure)
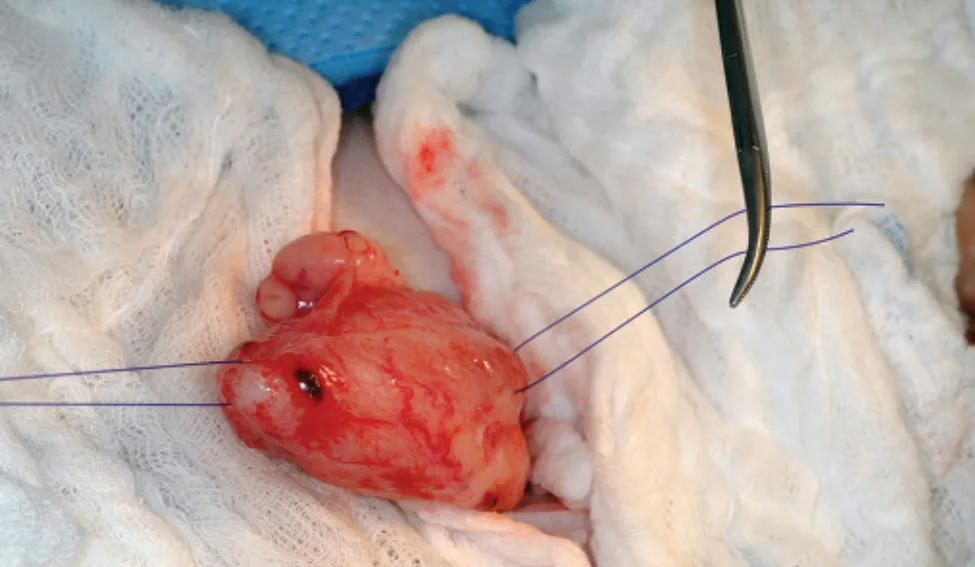
Isolate the bladder with laparotomy pads. If the bladder is overly distended, drain it by cystocentesis or passage of a urinary catheter. Identify an area of relatively low vascularity for the incision, and place full-thickness stay sutures proximal and distal to the planned cystotomy site.
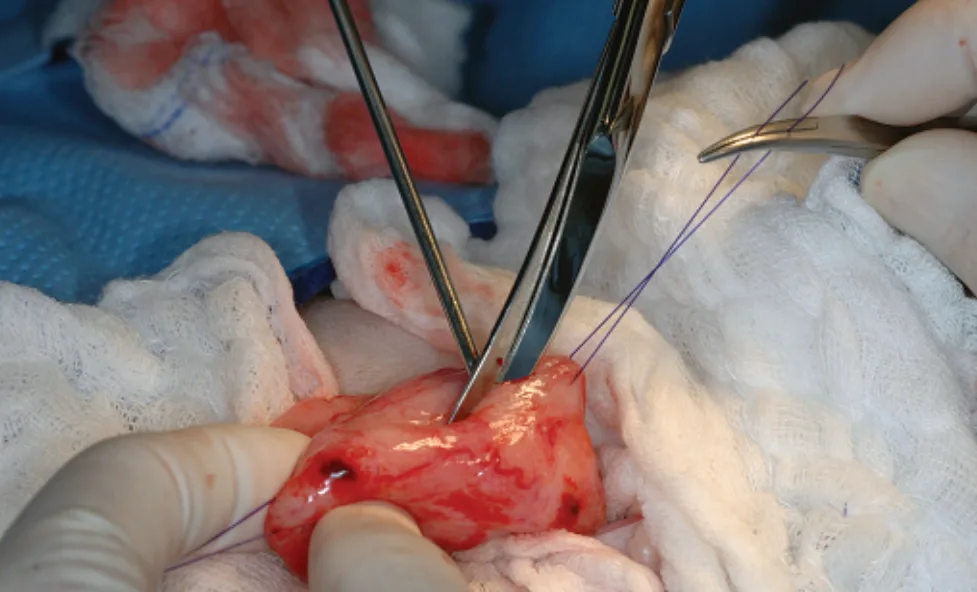
Using a scalpel blade, make a stab incision into the bladder between the stay sutures. Lengthen the incision as needed with Metzenbaum scissors or scalpel blade.
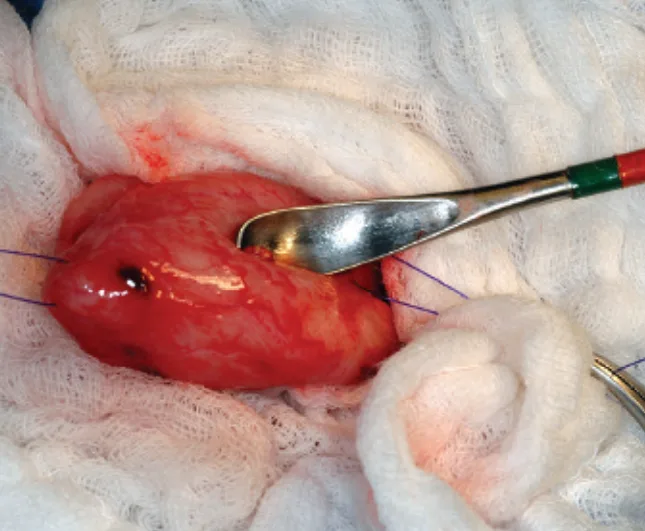
Remove large stones by grasping them with hemostats or forceps. Gently scoop out small stones with a bladder spoon.
Author Insight: Aggressive use of bladder spoons can prolong postoperative hematuria and patient discomfort.
If available, use a rigid scope to examine the inside of the bladder. Use retrieval baskets and grasping forceps to remove residual stones. Because this is a limited-approach cystotomy, a rigid scope facilitates complete examination of the bladder without the need for a full celiotomy.

Catheterize the urethra antegrade or retrograde (shown), and flush the urethra and bladder with sterile saline to remove debris, stones, or blood clots. Reexamine the interior of the bladder for additional calculi. Author Insight: Positioning cats in dorsal recumbency with the pelvic limbs pulled cranially permits concurrent cystotomy and perineal urethrostomy and can facilitate intraoperative catheterization.
Resect a full-thickness piece of tissue along the margin of the cystotomy for culture and sensitivity testing. Submit additional samples for histologic evaluation if abnormal tissue is present. It is advisable to take a bladder wall sample for culture from all cystotomy patients.
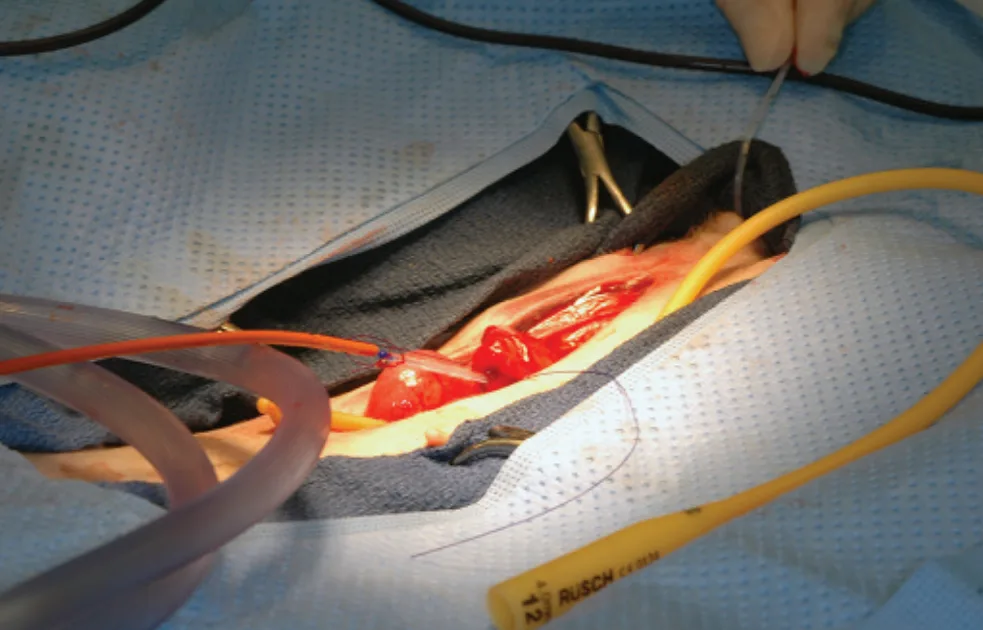
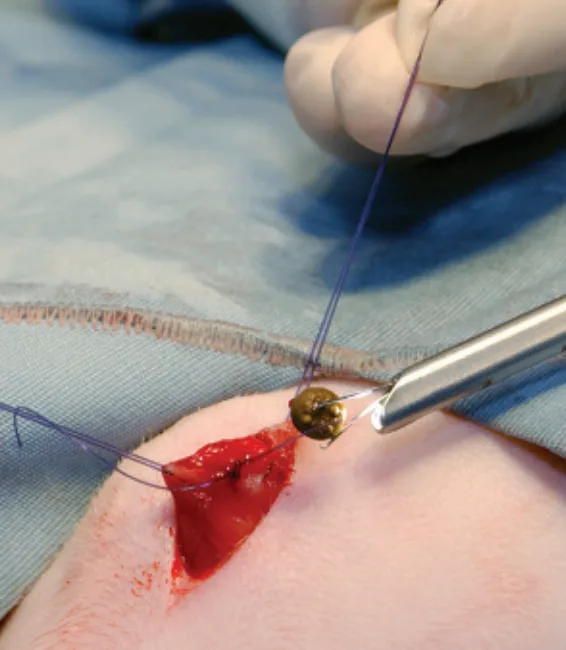
If postoperative urinary diversion is required, place a transurethral urinary catheter and/or transabdominal cystostomy tube. In female dogs, pass a red rubber or polypropylene catheter antegrade through the cystotomy and urethra and out the vulva, then suture its tip to a Foley catheter (retrograde catheter shown). Retract the catheters to pull the Foley catheter retrograde into the bladder.
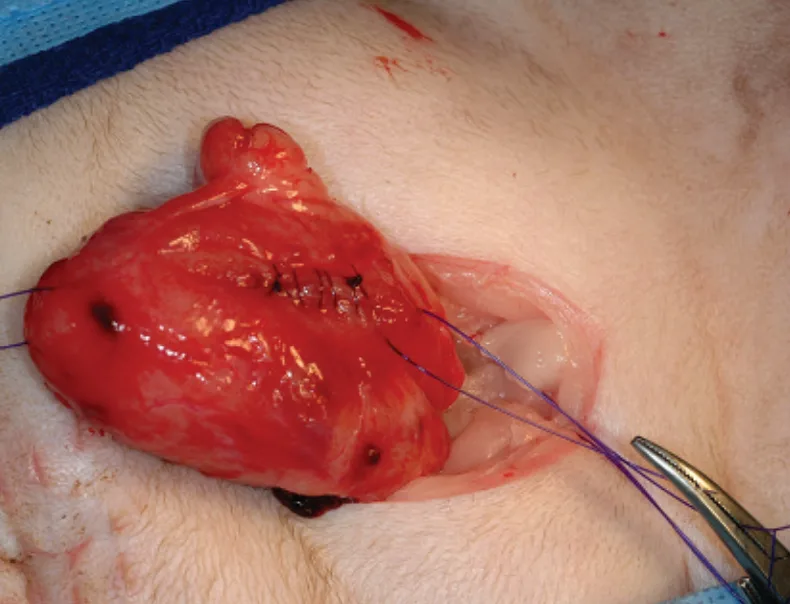
Close the bladder with a simple continuous pattern of synthetic, rapidly absorbable, monofilament suture, placing bites 3–5 mm apart, including submucosa but not mucosa. If desired, leak-test the bladder by inflating it with sterile saline through the urinary catheter or with a needle and syringe. Remove the stay sutures. Flush the abdomen with sterile saline if contamination has occurred. Tack omentum over the bladder if necrosis or leakage is a concern.