Emergency Stabilization for Transport

You have asked…
How can I safely prepare emergency patients for transportation to a 24-hour or referral facility?
The expert says…
Veterinary practitioners are often presented with a critically ill or injured patient requiring care or diagnostic testing that is unavailable at their clinic.
Considerations & Immediate Management
Stabilizing the ABCs (Airway, Breathing, Circulation), along with addressing pain, wounds and fractures, severe metabolic derangements, and neurological abnormalities, are paramount for safe transportation.
Related Article: Emergency Management of Spinal Cord Lesions
Airway
The airway may be compromised in many patients presented on emergency (see Upper Airway Obstruction Risks). If needed, supplemental oxygen (eg, flow-by, mask, collar, cage) can easily be administered. A mild sedative (eg, IV or IM butorphanol) may help alleviate signs such as marked increase in respiratory rate or effort, distress, and orthopnea (indicated by head and neck extension). If respiratory failure is imminent, rapid anesthetic induction with propofol, ketamine–benzodiazepine, or etomidate for endotracheal intubation and assisted ventilation with 100% oxygen is indicated until the underlying pathology is identified. Suction, swabs, or a stylet may assist with difficult intubations. Severe disease (eg, oropharyngeal trauma, obstructive upper airway disease; Figure 1) may make orotracheal intubation difficult, necessitating emergency tracheostomy.
Figure 1. Lilac discoloration of the tongue in a dog with partial upper airway obstruction; a pharyngeal hematoma was present from anticoagulant rodenticide ingestion.

Breathing
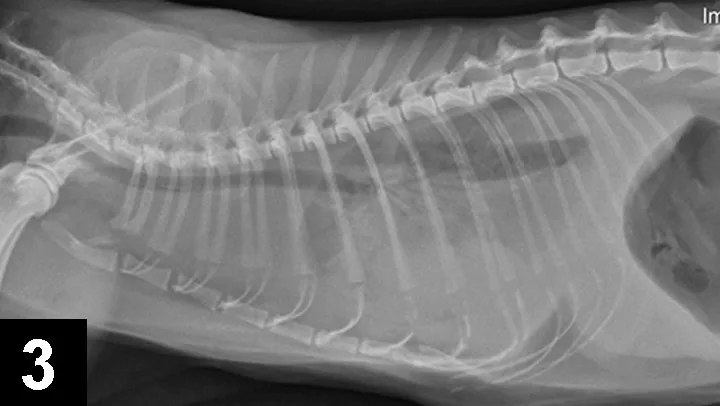
Many illnesses and injuries can impact normal oxygenation and ventilation. Stress, anxiety, and forced activity should be minimized. Pleural space disease (eg, pneumothorax, hemothorax, hydrothorax, pyothorax, chylothorax) can be identified by tachypnea, dull lung sounds with thoracic auscultation, open-mouth breathing, and a dyssynchronous respiratory pattern (ie, opposite motion of the chest and abdomen). Radiographs can identify pleural space disease (Figures 2 and 3) but should not be performed in cases with severe respiratory difficulty. If available, a quick ultrasound of the chest (thoracic-focused assessment with sonography for trauma [TFAST]) can readily identify pleural effusion and can be much less stressful and time consuming than radiography. Supplemental oxygen and thoracocentesis are always indicated.
If fluid is suspected in the pleural cavity, the thoracocentesis should be performed cranioventrally at the level of the costochondral junction bilaterally between the 2nd and 4th ribs. If pneumothorax is suspected, aspiration should be performed dorsocaudally between the 6th and 8th ribs. Butorphanol is typically well tolerated with respiratory distress and can facilitate thoracocentesis.
Related Article: Emergent Epilepsy & Status Epilepticus
Figure 2. Right lateral radiograph of a dog with pneumothorax; the arrow indicates the separation of the heart from the sternum.

Figure 3. Right lateral radiograph of a cat with hydrothorax secondary to heart disease. Note the loss of the cardiac silhouette and lack of normal lung fields.
Patients with suspected congestive heart failure should be administered injectable furosemide and topical nitroglycerin ointment. Severe cases of hypoxemia require intubation and manual ventilation with 100% oxygen.
Circulation
Hypoperfusion or shock can occur from hypovolemia (eg, GI or cavitary fluid or blood losses), cardiogenic shock (ie, the heart fails to function as a pump), obstructive shock (eg, gastric dilatation–volvulus [GDV], cardiac tamponade), or distributive disease (eg, sepsis, systemic inflammatory disease, severe metabolic or endocrine disease). Significant morbidity and mortality can occur if shock is not immediately addressed. Alterations in pulse quality, mucous membrane color, heart rate, capillary refill time, blood lactate, blood pressure, body temperature, and level of consciousness may indicate systemic hypoperfusion.
Related Article: When Every Second Counts: Emergency Preparation
Significant active hemorrhage should be addressed immediately with direct pressure, bandages, surgical ligation, cautery, and/or hemostatic agents (eg, gel foam, trauma gauze [kaolin impregnated]). Abdominal hemorrhage may also be slowed and intravascular volume improved with a pelvic limb or abdominal compression bandage. Emergent surgery for definitive hemostasis may be required.
Hypovolemic shock requires rapid IV infusion of fluids, accomplished with goal-directed therapy and aimed at normalizing vital signs. Low-volume resuscitation techniques (crystalloids, 10–20 mL/kg ± hydroxyethylstarch, 2–5 mL/kg) are used for patients with traumatic brain injury (TBI), acute hemorrhage, and pulmonary disease. Large-volume resuscitation (crystalloid, 30–50 mL/kg; hydroxyethylstarch, 5–10 mL/kg) can be used for dogs with massive fluid losses such as in sepsis, systemic inflammatory response syndrome (SIRS), severe gastroenteritis, GDV, anaphylaxis, or hypoadrenocorticism. These volumes should be administered over 10 minutes and the patient reassessed; these fluid doses can be repeated several times as directed by clinical status. Polymerized hemoglobin products may be considered in patients with hypotension and concurrent anemia. Hypertonic saline 7.5% (4 mL/kg) may be considered in patients that are not dehydrated and require lower-dose crystalloid resuscitation (eg, TBI); whole blood or packed RBCs may be necessary in patients with significant hemorrhage or anemia.
Upper Airway Obstruction Risks
Conditions that may result in upper airway obstruction and prompt an emergency tracheostomy include:
Brachycephalic syndrome
Foreign body obstruction
Granulomas or polypoid masses
Hypersensitivity (allergic) reaction
Laryngeal edema
Laryngeal paralysis
Neoplasia
Pharyngeal hematomas (trauma, coagulopathy)
Severe upper airway or facial trauma
Toxin ingestion (resulting in pharyngeal swelling)
Secondary Considerations & Additional Management
Electrolyte abnormalities are common in emergent patients. Hypokalemia may result in generalized muscle weakness and hypoventilation and can be treated with slow potassium chloride infusions; substantial hyperkalemia from renal or urinary disease (or hypoadrenocorticism if resulting in arrhythmias or hypotension) should be treated with calcium gluconate and insulin–dextrose ± sodium bicarbonate when associated signs (eg, alterations in heart rate, ECG, blood pressure) are present. Hypocalcemia is treated with calcium gluconate, and hypoglycemia should be treated with IV dextrose.
Steroids are rarely indicated with initial management, except with a hypoadrenocortical crisis or life-threatening inflammation (ie, leading to airway obstruction or status asthmaticus).
Status epilepticus should be addressed with injectable benzodiazepines, phenobarbital, levetiracetam, or propofol, as persistent seizures can lead to severe intracranial hypertension (as a result of cerebral edema) or hyperthermia. Patients with back or neck injuries should be transported in lateral recumbency on a solid surface (ie, stretcher) with restraint across the hips and shoulders to avoid further injury.
Fractures of the distal limbs should be stabilized with a bandage or splint to prevent further injury and pain. Penetrating objects should not be removed unless the clinician is prepared for immediate invasive surgery.
Wounds should be bandaged to prevent further injury and contamination; parenteral antibiotics may be initiated. Surgical treatment of wounds may be delayed with appropriate medical management until the patient is cardiovascularly stable.
Active cooling of patients with body temperatures >106°F (41°C) can be achieved by placing wet towels over the patient and directing a fan toward it, and/or applying alcohol to the axillary or inguinal regions; this can increase evaporative, convective, and conductive heat losses. For patients with temperatures <96°F (35°C), warming may be necessary; this may be accomplished with IV fluid line warmers, warm water blankets or blowers, and blankets placed around the patient.
Pain is exceedingly common in emergency cases, and the pain response can mimic shock or respiratory distress. Administration of systemic opioids is considered safe in most cases, rarely contributes to hypotension or respiratory compromise, and is essential for patients that have sustained significant trauma.
Preparing for Transport
Physical transportation of the patient should occur with as minimal stress as possible. Sedation or analgesia may be necessary, but medications that are reversible or short acting may be ideal if the patient is intended to be presented to a neurologist or surgeon. If there is potential compromise to the spinal cord, minimization of patient movement may be achieved via restraint on a flat, firm surface with duct tape or other restraint over the hips and shoulder. Patients should not be carried but transported on a large, moveable flat table (eg, gurney). Small patients may be transported in a small carrier with adequate ventilation to minimize stress.
GDV = gastric dilatation-volvulus, SIRS = systemic inflammatory response syndrome, TBI = traumatic brain injury, TFAST = thoracic-focused assessment with sonography for trauma
ANDREW LINKLATER, DVM, DACVECC, directs management of critical patients; performs advanced procedures; and provides lectures and instruction to students, interns, and residents at Lakeshore Veterinary Specialists in Glendale, Wisconsin. His interests include trauma, surgical emergencies, mechanical ventilation, and transfusion medicine. Dr. Linklater completed a residency in emergency and critical care at Animal Emergency Center in Milwaukee, Wisconsin, and an internship in Los Angeles. He graduated from University of Saskatchewan. Dr. Linklater has been published in journals and textbooks and has lectured nationally and internationally, including at the NAVC Conference.