Effusion in Cats
An 8-year-old, neutered male Himalayan cat presented to the veterinary clinic for respiratory distress of 2-days duration.
History. The distress was becoming worse; intermittent open-mouthed breathing had been noted by the owner. The cat was a strictly indoor cat and was current on vaccinations; he had no previous medical problems. The owner had no other pets.
Physical Examination. On presentation, the cat had moderate dyspnea and was tachypneic at 70 breaths/min. Mucous membranes were slightly pale; the heart was difficult to auscult on both sides. The abdomen did not appear distended and palpation was within normal limits.
The cat was given oxygen via a nasal oxygen mask. Because of the inaudible heart sounds, the clinician was suspicious of a pleural effusion. A lateral thoracic radiograph was done for confirmation. The radiograph showed separation of the lung borders from the thoracic wall and diaphragm as well as blurring of the cardiac silhouette and diaphragm. Pleural effusion was diagnosed.

A small area between the 7th and 8th rib space was clipped, and an 18-gauge, over-the-needle catheter was attached to a fluid extension set and 3-way stopcock. A 25-ml syringe was inserted to remove the fluid from the pleural space. A total of 100 ml was removed from the left side of the thorax and 60 ml was removed from the right side. A fluid sample was placed in both a purple-topped EDTA tube and a red-topped serum tube (see below for the gross fluid characteristics; see Figure 1 for fluid appearance). Direct smears and sediment smears of the fluid were made, and those slides along with the EDTA tube containing the fluid sample were sent to the local veterinary clinical pathologist for evaluation and interpretation. Making smears at the clinic allows interpretation of the fluid sample in the event of sample degradation or artifacts that may occur during transport to the laboratory.
Fluid Analysis
Source: Pleural fluid—1 sample in a purple-topped EDTA tube and another in a red-topped serum tube
Color: White
Color of supernatant: White
Clarity: Opaque
Total nucleated cells/μl: 3600
Red blood cells/μl: < 100,000
Total protein (g/dl): 5.0—turbidity of the sample interferes with an accurate assessment of TP read by refractometry
Differential cell count: 93% small mature lymphocytes,
5% monocytes, 2% nondegenerative neutrophils
Ask yourself ...
Is the fluid a transudate, modified transudate, or exudate?
Can you characterize the category of the fluid further?
What other tests should be run?
What is the cause of the effusion?
Diagnosis: Chylous effusion; modified transudate

Chylous effusion is a milky-white fluid that fails to clear on centrifugation. These fluids are made of chyle, an admixture of lymph and chylomicrons. The latter primarily comprise triglycerides. They are derived from dietary lipids absorbed from the intestine and are transported to the lymphatics and then to the venous circulation (via the thoracic duct) for distribution into tissues. As a result, chylous effusion is expected to have a high triglycerideand a low or normal cholesterol content compared with serum and a cholesterol-to-triglyceride ratio less than 1. Pseudochylous effusion is rare in veterinary medicine; it is similar in color to chylous effusion and is secondary to chronic inflammation. In addition, pseudochylous effusion is clear on centrifugation, has increased cholesterol content, and has decreased-to-normal triglyceride content.
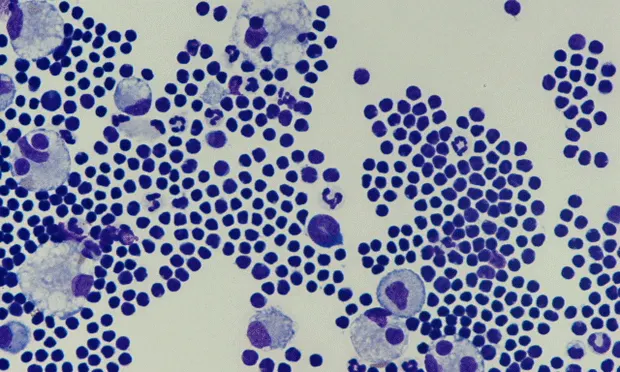
Figure 2. Cytocentrifuge preparation smears of the fluid (A original magnification x 200; B original magnification x500)
Chylous effusion in cats has many causes and is found more often in the thorax than in the abdomen. Effusion is secondary to functional or physical lymphatic obstruction. Possible differentials include the following:
Cardiomyopathy
Heartworm disease
Lymphangiectasia
Mediastinal neoplasia (lymphoma/thymoma)
Trauma or rupture of the thoracic duct
Mesenteric root tumor.
Ultrasonographic evaluation can often provide additional information, but many cases are idiopathic. Animals may have a history of dyspnea or coughing. Physical examination findings may include the following:
Decreased heart and lung sounds
Arrhythmia
Murmur
Increased jugular pulses with right-heart failure
Decreased compressibility of the anterior thorax in cats with neoplasia.

Other fluid characteristics include predominant small, mature lymphocytes acutely (modified transudate); increased neutrophils chronically (modified transudate/exudate); or the presence of immature lymphocytes in cases of lymphoma. The increased percentage of neutrophils associated with chronic chylous effusion is believed to be caused by the irritating nature of chyle on the pleural/peritoneal lining, secondary to inflammation induced by multiple thoracocenteses or abdominocenteses (Figure 3) and possible iatrogenic infection as a result of such procedures. The cat in this case had evidence of hypertrophic cardiomyopathy and secondary chylous effusion as a result of functional lymphatic obstruction resulting from cardiac insufficiency.
Figure 3. Chronic chylous effusion. Note the presence of neutrophils admixed with the small mature lymphocytes. Foamy-appearing, lipid-filled macrophages are a common finding in chylous effusion (original magnification x 500).
Did You Answer ...
The fluid is a modified transudate (TP 2.5 to 5.0 g/dl and TNCC < 10,000 cells/ml). Transudates have a TP concentration less than 2.5 g/dl and a TNCC less than 1500 cells/ml. Exudates have a TP concentration greater than 3.0 g/dl and TNCC greater than 10,000.
The predominant small, mature lymphocytes and the white color of the fluid and supernatant are compatible with chylous effusion. An increased percentage of neutrophils will occur as the effusion becomes more chronic, with frequent thoracocentesis, and possibly with iatrogenic infections resulting from thoracocentesis. Typically, neutrophils in chronic chylous effusion are nondegenerative. Degenerative neutrophils may signal a concurrent septic process.
Comparison of fluid cholesterol and triglyceride levels to serum provides a definitive diagnosis of chylous effusion if cytologic fluid evaluation cannot readily be done. However, the cause may be missed (i.e., neoplasia) if cytologic evaluation is not performed.
The chylous effusion may be secondary to a functional or physical lymphatic obstruction or may be idiopathic.
Physiochemical Characteristics of Chylous Effusion
Physical characteristics: Milky to white-pink, turbid to opaque
Protein concentration: Interference with the lipid for accurate determination
TNCC: Variable, but often < 10,000 cells/ml.
Cell types: Lymphocytes predominate in acute cases; neutrophils can predominate in chronic cases
Special stains: Sudan-positive, which stains lipid droplets present in chylous effusion
Biochemical properties: Triglycerides of fluid greater than serum triglyceride and cholesterol content less than serum cholesterol
TP = total protein; TNCC = total nucleated cell count