Ear Mass in a Dog
An 8-year-old spayed female Boston terrier was presented for examination of a mass on the right ear.
History. The owner first noticed the mass 2 months ago; it had doubled in size since then.
Physical Examination. The dog had a 1 cm × 1 cm mass on the dorsal aspect of the base of the right ear. The mass was firm, dome-shaped, alopecic, pink, and nonpainful on palpation. No other cutaneous masses were noted; however, the right superficial cervical lymph node was mildly enlarged.
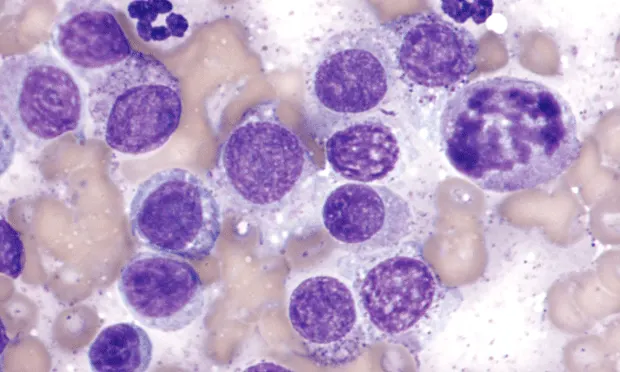
Diagnostics. Fine-needle aspirates of the ear mass (Figure 1) and the right superficial cervical (prescapular) lymph node (Figure 2) were collected.
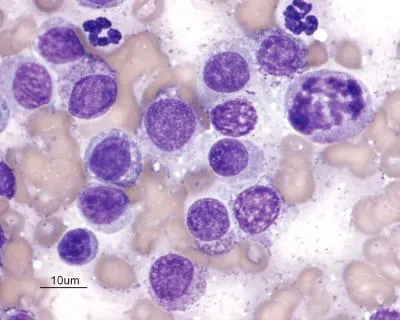
Figure 1.
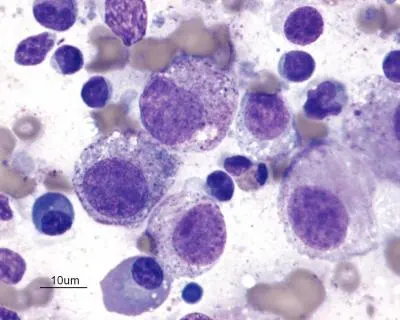
Figure 2.
Diagnosis:Poorly differentiated mast cell tumor with metastasis to the prescapular lymph node
Mast cell tumors (MCTs) are the most common cutaneous tumors in dogs, accounting for 16% to 21% of all cutaneous tumors. The incidence is increased in boxers, Boston terriers, Labrador retrievers, beagles, and schnauzers.1 Although a diagnosis of MCT can usually be made cytologically, the biological behavior of these tumors varies widely. The histologic grade (typically determined from formalin-fixed, hematoxylin and eosin–stained tissue sections) is the most valuable prognostic indicator of survival, metastasis, and disease-free interval. Consequently, excisional biopsy with histopathologic examination is always indicated.1
Tumor Grading. The most widely used histologic grading system differentiates tumors into the following grade categories:• Grade 1 tumors: Well-differentiated, low-grade tumors with a good prognosis (reported metastatic rate < 10%)• Grade 2 tumors: Moderately differentiated, with a cautionary prognosis (reported metastatic rates up to 22%)• Grade 3 tumors: Poorly differentiated, with the poorest prognosis (reported metastatic rate, 55% to 96%).2
Application of this histologic grading system provides valuable prognostic information (especially for grade 1 and 3 tumors); however, the prognosis for grade 2 tumors is uncertain. Research is being conducted to identify prognostic indicators that might enable consistent recognition and subcategorization of less aggressive and more aggressive grade 2 tumors (called grade 2a and grade 2b, respectively, by some pathologists).
Cellular Proliferation. Assessments of cellular proliferation indicators (eg, mitotic index, Ki-67, proliferating cell nuclear antigen immunostaining, and argyrophilic nucleolar organizing region histochemical staining) help determine the aggressive nature of the tumor. If cell proliferation is high, the tumor is deemed more aggressive.3
One study showed a strong correlation between the mitotic index (number of mitotic figures seen in 10 high-power [400×] fields) and tumor grade, and this can be a valuable tool to help identify grade 2 tumors that are more likely to metastasize. Tumors that have a mitotic index greater than 5 were associated with an extremely short median survival time compared with those with a mitotic index less than 5.3
Evaluation for the presence of a mutation in the c-kit protooncogene may also be helpful; c-kit juxtamembrane domain mutations are often associated with tumors of a higher histologic grade (ie, aggressive grade 2 and 3 tumors).3
Tumor Staging. The Table shows the World Health Organization (WHO) clinical staging system for canine MCTs. MCTs generally metastasize to regional lymph nodes first and then to the spleen, liver, mesenteric lymph nodes, and bone marrow.1 Consequently, after the initial diagnosis of a cutaneous MCT, fine-needle aspiration of the regional lymph node that drains the tumor site is always recommended, even if the node is not obviously enlarged. The decision to conduct further clinical staging procedures should be based on whether one or more of the following criteria are met:• Regional lymph node metastasis is evident.• Histopathologic assessment determines the tumor to be grade 2 or grade 3.• Surgical margins are incomplete, and more aggressive or costly treatment of the primary site is being considered.1
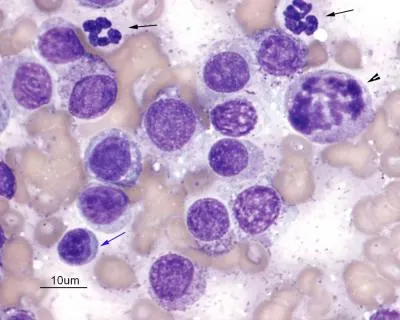
Figure 1. Neoplastic mast cells in the ear mass aspirate. Fourteen poorly granulated mast cells, 2 segmented neutrophils (black arrows), 1 small lymphocyte (blue arrow), and many erythrocytes arepresent. Note the moderate anisocytosis and anisokaryosis of the mast cells. A mitotic figure is present in 1 mast cell (arrowhead).Modified Wright’s stain; magnification, 1000×
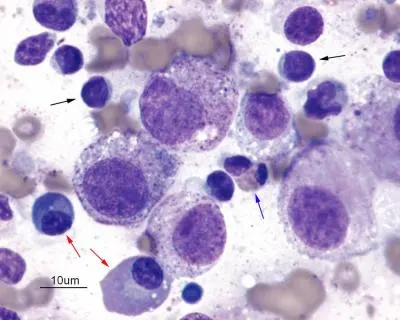
Figure 2. Neoplastic mast cells in the superficial cervical lymph node aspirate. Note the poorly granulatedmast cells that have marked anisocytosis and marked anisokaryosis. There are also small lymphocytes(black arrows), an eosinophil (blue arrow), and 2 plasma cells (red arrows), suggesting reactive lymphoid hyperplasia within the node. Numerous erythrocytes are also present. Modified Wright’s stain; original magnification, 1000×
If further staging is required, abdominal ultrasonography should be performed with cytologic assessment of lymph nodes, spleen, or liver if warranted. Bone marrow involvement is unlikely in the absence of disease in the regional lymph nodes or abdominal organs.1 Although metastases to the lungs are rare, thoracic radiography is indicated as part of a thorough staging procedure.
Outcome. The cutaneous ear mass and enlarged superficial cervical lymph node were excised and submitted for histopathologic examination. The ear mass was diagnosed as a grade 2 MCT, and metastasis to the superficial cervical lymph node was confirmed. Results of complete blood count and serum biochemical analyses were unremarkable; however, 3 mast cells were seen during a buffy-coat examination.
Generalized splenomegaly was evident during abdominal ultrasonography and a marked splenic mast cell infiltrate was confirmed cytologically. Finally, a bone marrow aspirate included a marked infiltrate of neoplastic mast cells (Figure 3). Further diagnostic methods and treatment options were not pursued because of the grave prognosis.
Ask yourself…
• What are your interpretations of the cells seen in the fine-needle aspirates of the ear mass and lymph node?
• What is the cytologic diagnosis?
• What additional tests are indicated?
Diagnosis:Poorly differentiated mast cell tumor with metastasis to the prescapular lymph node
Q • What are your interpretations of the cells seen in the fine-needle aspirates of the ear mass and lymph node?
A • Aspirates of the ear mass were primarily comprised of individual round or oval mast cells and many erythrocytes (Figure 1). Mast cells had moderate anisocytosis and moderate anisokaryosis, and they varied from nongranulated to poorly granulated. Mitotic figures were common in the sample. Occasional neutrophils and small lymphocytes were also present.
Aspirates of the superficial cervical lymph node included a similar population of neoplastic mast cells, although there was a greater degree of anisocytosis and anisokaryosis (Figure 2). Along with the normal population of lymphocytes, plasma cells were proportionately increased, suggesting secondary reactive lymphoid hyperplasia. Mild infiltration of eosinophils (a common finding seen with mast cell tumors) was also noted.
Q • What is the cytologic diagnosis?
A • Cytologic diagnosis is a poorly differentiated mast cell tumor with metastasis to the right superficial cervical lymph node.
Q • What additional tests are indicated?
A • Thorough clinical staging for disseminated mastocytosis is indicated and should include the following:
Complete blood count with thorough examination of the blood smear and possibly buffy-coat preparation to search for peripheral mastocytosis
Abdominal ultrasonography and, if warranted, cytologic assessment of mesenteric lymph nodes, spleen, and liver
Bone marrow aspiration with cytologic assessment performed by a clinical pathologist; and
Thoracic radiography.1
In our opinion, the buffy-coat preparation is unnecessary if other staging procedures, such as abdominal ultrasonography with cytologic assessment of spleen, liver, lymph nodes, and bone marrow are performed.
EAR MASS IN A DOG • Bradley Galgut & Lisa Pohlman
References1. Mast cell tumors. Thamm DH, Vail DM. In Withrow SJ, MacEwen EG (eds): Small Animal Clinical Oncology, 4th ed—Philadelphia: WB Saunders, 2006, pp 402-424.2. Clinical management of mast cell tumors in dogs. Gieger T, Northrup N, Wall M. Compend Contin Ed Pract Vet 27:56-68, 2005.3. Mitotic index is predictive for survival for canine cutaneous mast cell tumors. Romansik EM, Reilly CM, Kass PH, et al. Vet Pathol 44:335-341, 2007.4. Effects of stage and number of tumours on prognosis of dogs with cutaneous mast cell tumours. Murphy S, Sparkes AH, Blunden AS, et al. Vet Rec 158:287-291, 2006.
Impact of tumour depth, tumour location and multiple synchronous masses on the prognosis of canine cutaneous mast cell tumours. Kiupel M, Webster JD, Miller WR, Kaneene JB. J Vet Med 52:280-286, 2005.6. Advances in the diagnosis and management of cutaneous mast cell tumours in dogs. Dobson JM, Scase TJ. J Small Anim Pract 48:424-431, 2007.