The Concept of Corneal Protection
Corneal protection entails covering, or shielding, the cornea from injury or exposure. It also involves maintenance of status or integrity. When corneal protection is considered clinically, all tissues involving the orbit, eyelids, conjunctiva and nictitans, lacrimal gland tear production, and drainage system contribute to the cornea’s well-being and must be evaluated.
In purebred dogs, outer eye diseases and corneal protection issues are often associated with inherited predisposing abnormalities, such as shallow orbits, exophthalmos, lagophthalmia, entropion and ectropion, and keratoconjunctivitis sicca (KCS). In cats, inherited predisposing abnormalites are less frequent but include exophthalmos and entropion in the brachycephalic breeds. Infectious diseases in cats seem to play a more frequent role than inherited diseases in corneal protection issues.
The cornea can be conveniently examined with good magnification and illumination. Inspection of the outer eye occurs during presentation for diagnosis and also following medical and surgical therapies. The cornea is quite resilient and, despite significant challenges to its clarity and integrity, often responds successfully to treatment, thereby maintaining vision.
Diagnostics
The accessibility of the cornea permits many different types of diagnostic analysis, most of which can be performed in the examination room.
Eyelid Function
Eyelid function can be determined by observing the rate and quality of blinking, the interrelationships between the lids and conjunctivae, and the presence of any eyelid abnormalities. Both corneal and conjunctival sensation via the ophthalmic division of the trigeminal nerve is essential for precorneal tear film health. Likewise, innervation by the palpebral branch of the facial nerve is essential for orbicularis oculi muscle action and the palpebral reflex.
Corneoconjunctival protection is in jeopardy when sensation and lid mobility are impaired. Normal dog and cat blink rates are 3 to 12 blinks per minute and 1 to 3 blinks per 5 minutes, respectively. These blinks are often (up to 70%) incomplete. Blinks in both species often occur in both eyes simultaneously, and excited animals may blink excessively (most likely due to excessive sympathetic tone). Evaluation of the palpebral reflex response not only includes presence or absence of the response; but also evaluation of the speed, rigor, and ability to maintain closure of the lids. Diseases that affect blinking are often slow in onset; both speed and extent of blinking are gradually affected before total loss of function results. Both the dazzle reflex and menace response can also help determine eyelid function.
Corneal Sensitivity
Corneal sensitivity is most often tested by touching the cornea and/or conjunctiva with a cotton wisp while holding the eyelids open. The swab’s tip must be small and the cornea touched from the lateral side to decrease likelihood of a menace response. A positive sensitivity response is retraction of the globe and protrusion of the nictitans.
The Cochet-Bonnet esthesiometer is an improved method for not only detecting but also quantifying sensitivity of the cornea in its different quadrants and center. This device, shaped like a fountain pen, has an adjustable semitransparent fiber protruding from its end, which helps determine the level of corneal sensation. The shorter the protruding filament that induces a response, the less sensitive the cornea.
Brachycephalic dogs and cats, diabetic animals, older animals, and foals appear to have decreased corneal sensitivity. In brachycephalic dogs, the central corneal sensitivity is reduced, which combined with a thin central precorneal tear film, may predispose these breeds to central corneal ulceration.
Corneal & Conjunctival Health
To evaluate the corneal and conjunctival health, several diagnostics can be employed, based in part on the 3 different layers of the precorneal tear film; this film covers not only the entire outer cornea but also the palpebral and bulbar conjunctivae and nictitans surfaces.
Fluorescein StainingThe lipid outer layer is evaluated by tear break-up time (BUT). With this technique, fluorescein stain is applied to the dorsal bulbar conjunctiva while holding the eyelids open and observing the corneal surface with a cobalt blue light source and magnification. The time for the development of dry spots in the tear film is the BUT. Normal BUT in the dog is 20 ± 5 seconds and in the cat, 17 ± 4 seconds.
In addition, application of fluorescein stain during the ocular exam allows corneal evaluation. During this test, the stain is applied to the dorsal bulbar conjunctiva from a moistened dye strip and is distributed across the cornea by the patient’s eyelids. Evaluation of fluorescein retention should occur immediately thereafter, as the dye can rapidly traverse the exposed corneal stroma and enter the anterior chamber. Since damaged corneal epithelium or recently reattached epithelium may stain very faintly, close observation of the corneal surface with magnification and a cobalt blue light is essential. The cornea should be rinsed following application of fluorescein to prevent false positives due to stain pooling.
Schirmer’s Tear Test (STT)The aqueous layer is tested by STT 1 and 2. STT 1 measures both reflex and basal tear secretion; however, it only measures the aqueous fraction of the tear film. Normal range (mean ± SD) in dogs is 18 to 24 ± 4 to 5 mm wetting/minute in dogs; in cats, it is 14 to 17 ± 5 to 6 mm. Values are more variable in cats; some have low values and no ocular disease.
For STT 2, topical anesthesia is applied and the conjunctival sac is dried with a Dacron swab; test paper is inserted into the conjunctival fornix of the mid lower lid for 1 minute. This test estimates only basal tear secretion. STT 2 in the dog ranges from 3.8 ± 2.7 to 13.95 ± 4 mm wetting/minute; in cats it is 80% of the STT 1 levels.
As the most frequent cause of secondary conjunctivitis, KCS in dogs is associated with aqueous tear deficiency. Routine use of STT is important in diagnosing early disease, when medical therapy is most successful. Ocular irritation can artificially increase STT rates; therefore, this test should be employed early in the ophthalmic examination. Although measurements can be affected by the type of tear test paper, season, time of day, and perhaps other factors, these differences are generally 1 mm wetting/minute or less and not clinically significant.

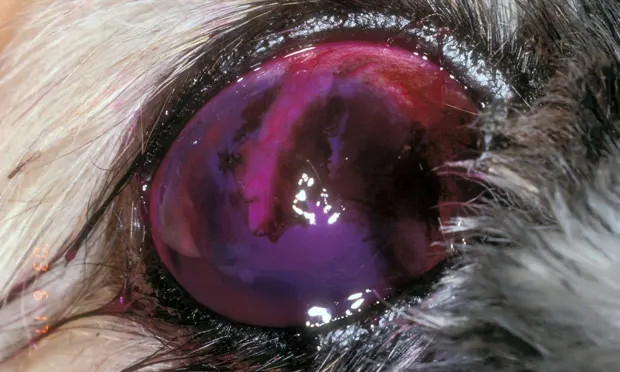
Rose Bengal StainingThe mucoid or deep layer of tear film may be evaluated by the retention of rose bengal stain (Figure 1. Generalized corneal epithelial rose bengal retention in an eye with lagophthalmia, previous descemetocele, and pedicle conjunctival graft).
Corneal Protection
Medical Protection
Several ophthalmic drugs are available for either short- or long-term corneal protection. However, the most effective drugs are those that stimulate aqueous tear formation rates due to their longer duration of action. Animals with concurrent corneoconjunctival disease are the most frequent candidates for these drugs.However, other patients, such as young brachycephalic dogs with previous bilateral corneal ulcerations, brachycephalic dogs with only one eye, and those with central rose bengal stain retention and low-normal STT rates (about 10 mm wetting/minute) are also candidates.
Current topical drugs that may increase STT 1 levels include cyclosporine, tacrolimus, and pimecrolimus in patients with KCS. Drug concentrations, frequency of instillation, and stage of KCS may affect drug efficacy. If one drug fails to adequately increase tear formation rates and resolve clinical signs, increased drug concentration, more frequent administration, and/or switching to another drug must be considered. Generally, once KCS is diagnosed, long-term therapy is indicated. Delayed or intermittent topical therapy may allow immune-mediated dacryoadenitis to advance, promote greater gland destruction, and decrease future drug efficacy.
Tear replacements (both liquid and ointments) can provide corneal protection; however, since their contact times vary from minutes to a few hours, their benefits are limited. Generic mineral oil ointments have the longest corneoconjunctival contact times. In humans, vision blurring is a major problem, but in animals this appears less important.
Medical corneal protectors tested experimentally include biogradable tear inserts and lacrimal punctal implants (or plugs) that increase tear formation rate by either increasing available tears or preventing tear drainage. Other devices include collagen shields and contact lenses. Some of these devices may also serve as reservoirs to release medications over time.
Surgical Protection
There are several surgical eyelid procedures that promote corneal protection. In some patients, these are the most cost-effective and long-term methods to protect either at-risk or diseased corneas (Table 1). Brachycephalic breeds and breeds with macropalpebral fissures often benefit from surgical procedures that reduce the size of the palpebral fissure and promote improved central corneal protection. For neurotrophic and neuroparalytic keratitis associated with reduced trigeminal and facial nerve function respectively, either temporary or permanent partial lateral tarsorrhaphy may be beneficial. Loss of the ability to blink can be devastating to normal corneas, and this procedure can protect the cornea during nerve recovery.
There are several medial and lateral permanent tarsorrhaphy techniques that reduce corneal exposure in breeds susceptible to repeated central corneal ulceration secondary to reduced central corneal sensitivity, lagophthalmia, and corneal microtrauma. These techniques are most useful in young brachycephalic breeds as well as senior dogs with active, bilateral corneal disease. In certain breeds, resection of the nasal folds is combined with medial canthoplasty to reduce medial canthus trichiasis, entropion, and overall size of the palpebral fissure.
Nictitating membrane flaps and temporary complete tarsorrhaphies, used infrequently now, also offer short-term corneal protection. Correct suture placement and possible suture readjustment several days after initial placement are critical to prevent direct contact between the suture and cornea and subsequent corneal ulceration. Conjunctival graft procedures can also be used for long-term treatment of severe corneal ulcerations.

Protection for At-Risk Corneas
Medical, surgical, or a combination of these therapies may be used when serious insult and potential corneal damage are anticipated.
A temporary partial tarsorrhaphy protects the entire cornea but still allows application of medications to the eye after traumatic proptosis, maintains the globe within the orbit, and protects the cornea from exposure until a normal palpebral reflex returns (Figure 2).Figure 2. Complete temporary tarsorrhaphy after traumatic proptosis is necessary to maintain the globe within the orbit and protect the cornea. Preoperative appearance: (A) Imeddiate postoperative appearance (B).
A temporary tarsorrhaphy can be performed after evisceration with insertion of an intraocular prosthesis. The scleral incision for the removal of the intraocular tissues and insertion of the silicone sphere reduce corneal sensitivity and increase the possibility of postoperative central corneal ulceration. Medications may be administered on either side of the tarsorrhaphy.

After trauma and following ocular surgery, a temporary or even permanent partial tarsorrhaphy can be employed when either the trigeminal nerve or branches of the facial nerve are damaged and corneal protection is critical. The central cornea is generally most vulnerable.
The central cornea in the brachycephalic dog often has reduced corneal sensitivity, thinner than normal precorneal tear film, lagophthalmos, and medial canthal trichiasis. When these dogs are evaluated with topical fluorescein and rose bengal, there is faint retention in the central cornea, signaling that the epithelium in this area is abnormal. If the dog has a history of previous corneal ulcerations, it may benefit from drugs that increase STT 1 levels or surgery, such as medial canthoplasty, to reduce the palpebral fissure and enhance corneal protection (Figure 3).
Figure 3. Postoperative appearance of a medial canthoplasty in a pug. The palpebral fissure size is reduced to treat bilaterial lagophthalmia.


Protection for Diseased Corneas
Medical, surgical, or a combination of these therapies are also used when corneal disease is already present, including such conditions as corneal erosions/ulceration or sequestrum formation.


Corneal protection is often initiated for corneal erosions (to control pain and enhance epithelial attachment) and deep stromal corneal ulcerations (to strengthen the cornea and prevent perforation, Figure 4).
Figures 4a-d. Examples of pedicle bulbar conjunctival grafts in dogs: Graft used to repair a perforated corneal ulcer and Iris prolapse. (A). Use of the pedicle bulbar conjunctival graft for a central descemetocele (B); preoperative appearnce (note the bulging descemetocele, C); postoperative appearance of eye in C at 40 days, just before the pedicle is transected (D).
There are many different strategies available to repair corneal defects (Table 2). The goal of these repairs is to achieve a transparent or nearly clear cornea. In humans, deep or full-thickness keratoplasty is often used; in animals, conjunctival grafts are most often used. New methodologies in small animals include amniotic membrane transplantation and porcine small intestinal submucosa grafts; these methods offer promise of greater corneal transparency postoperatively in many patients.