Common Gastrointestinal Signs = Challenging Diagnosis?
A 6-year-old spayed female mastiff dog was presented with a 2-week history of inappetence and diarrhea.
History. The owner had been out of town for 2 weeks, during which time the caretaker reported that the dog had a poor appetite and several episodes of diarrhea. The owner had noticed significant weight loss (about 10 kg) over the last several months and intermittent loose stool. There were no reports of polyuria, polydipsia, vomiting, or coughing. Current medications include heartworm and flea preventatives.
Physical Examination. The dog was quiet, alert, responsive, and hydrated. The temperature, heart rate, and respiratory rate were within normal limits. The body weight was 62.8 kg with a body condition score of 3-4/9. The only abnormalities were thin body condition and generalized loss of muscle mass. Findings on rectal and fundic examinations were unremarkable.
Diagnostics. Table 1 shows results of routine blood analysis. Urinalysis was within normal limits.
Diagnosis: Addison's Disease
Clinicopathologic Abnormalities.The complete blood count indicates mild, regenerative anemia consistent with blood loss or hemolysis. Although the total WBC is within the reference range, the WBC differential shows a high-normal lymphocyte count, eosinophilia, and a neutrophil count within the reference range. The finding of a normal or increased lymphocyte or eosinophil count in a stressed or ill dog should raise suspicion for Addison's disease. However, the eosinophil or lymphocyte numbers are not sensitive or specific and are used only as a hint to adrenocortical health.
Serum biochemistry analysis revealed mild hypoalbuminemia, marked hypocholesterolemia, and a discordant BUN:creatinine ratio (35 [normal, approximately 20]). The discordant BUN:creatinine ratio suggests gastrointestinal blood loss; it may also be due to a high-protein diet (which causes an elevated BUN level), or cachexia, which causes decreased creatinine concentration. The regenerative anemia, without evidence of hemolysis, is also consistent with blood loss.
Differential Diagnoses.The primary differential diagnoses include primary bowel disease (including inflammatory bowel disease, lymphangiectasia, neoplasia, and infectious causes), metabolic disease (Addison's disease), and possibly liver disease.
Hypocholesterolemia can be due to severe bowel disease (loss of proteins including lipoproteins; eg, lymphangiectasia), liver dysfunction (decreased production), and Addison's disease (multifactorial; mechanism poorly understood). The many causes of hypoalbuminemia include protein-losing enteropathy, protein-losing nephropathy, liver dysfunction (decreased production), Addison's disease (multifactorial), blood loss, acute negative-phase protein (eg, as in inflammatory disease), and vasculitis.
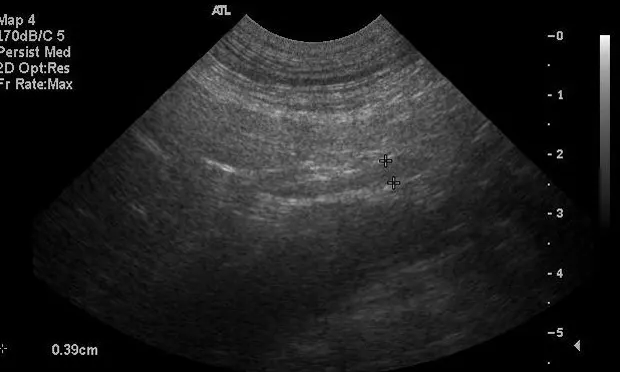
Diagnostics. Abdominal ultrasonography was performed to assess the gastrointestinal tract, liver, and adrenal glands (Figures 1 and 2). The gastrointestinal tract and liver were unremarkable; both adrenal glands were mildly decreased in size (maximum width of left and right adrenal glands, 0.38 cm and 0.39 cm, respectively [normal, 0.5-0.8 cm]). Bile acids were within the reference range (preprandial, 2 µmol/L; postprandial, 6 µmol/L).Results of fecal flotation, fecal direct smear, and a heartworm test were negative.
An ACTH stimulation test is the gold standard for Addison's disease. This test was performed and the results are listed in Table 2. An inadequate response to the ACTH stimulation test (ie, post-ACTH plasma cortisol level < 2 µg/dL) is diagnostic for hypoadrenocorticism (Addison's disease).
This dog had normal serum electrolyte (sodium, potassium) levels, indicating adequate mineralocorticoid function. Thus, the subnormal post-ACTH cortisol level, along with normal electrolytes, was diagnostic for glucocorticoid-deficient hypoadrenocorticism. This is an uncommon form of Addison's disease in dogs and is more challenging to diagnose. Clinical signs and clinicopathologic abnormalities are nonspecific. Anemia, normal or increased lymphocyte and eosinophil count, hypocholesterolemia, and hypoalbuminemia in dogs with chronic clinical signs related to gastrointestinal disease may warrant an ACTH stimulation test before other, more invasive testing.
Treatment. The dog was prescribed oral prednisone based on the diagnosis of glucocorticoid-deficient hypoadrenocorticism. Desoxycorticosterone pivalate was not given because the dog had normal serum electrolytes (sodium, potassium), suggesting adequate mineralocorticoid function. Prednisone was initially started at 0.5 mg/kg per day (30 mg) and ultimately decreased to 0.1 mg/kg per day (5 mg); the goal of therapy was a good appetite (without evidence of polyphagia, polyuria, or polydipsia) and no evidence of vomiting, diarrhea, weakness, or depression.
Outcome. Follow-up serum biochemistry analyses 2 weeks after prednisone therapy showed resolution of hypocholesterolemia and hypoalbuminemia along with continued normal serum electrolyte concentrations. Monitoring of serum electrolytes was recommended once every 2 or 3 months, or sooner if abnormal clinical signs such as weakness, lethargy, or a decreased appetite occurred. The dog gained 12 kg in 4 weeks and had good appetite, adequate activity level, and resolution of diarrhea.