Clinical Suite: MRSP Infections in Dogs & Cats
Alexander Werner Resnick, VMD, DACVD, Animal Dermatology Center
Christopher Keller, Animal Dermatology Center, Studio City, California
Overview
Alexander Werner, VMD, DACVD, Animal Dermatology Center, Studio City, California
Superficial bacterial folliculitis, or pyoderma, is common in dogs, uncommon in cats, and most often a secondary disease. Signs vary widely and reflect the underlying cause (eg, allergic skin disease, endocrinopathy).
The initial lesion of pyoderma is the pustule leading to the crusted papule. Similar in appearance to a pebble cast into calm water, individual lesions increase into ever-expanding circular areas with peripheral crusts, erythema, and central clearing (ie, the epidermal collarette). Multiple crusted patches with erythema and malodor eventually develop.
Related ArticleMRSA & MRSP at a Glance
Staphylococcus pseudintermedius is the primary bacterium isolated in superficial bacterial folliculitis. It is frequently a resident of the nares, lip folds, and anal region of dogs, and a transient on the haircoat. Infection by S schleiferi and S aureus is less common. Canine infection with S aureus—particularly methicillin-resistant S aureus (MRSA)—is often associated with exposure to a human in the household with MRSA or frequent visits to healthcare facilities. S aureus and S pseudintermedius are cultured with similar frequency from the skin of healthy cats and cats with inflammatory skin disease, although the frequency of culturing methicillin-resistant strains is low.
TREATMENT
Treatment of pyoderma caused by methicillin-resistant S pseudintermedius (MRSP) differs little from that for methicillin-sensitive S pseudintermedius (MSSP) infection, except for the need to correctly identify the appropriate antibiotic that should be prescribed. Culture and sensitivity testing are recommended in cases of pyoderma that fail to respond to empiric choice antibiotics.
Treatment for MRSP-related pyoderma must include topical antibacterial therapy, systemic antimicrobials, and identification and management of any underlying process that permitted infection from MRSP colonization.
Patients with pyoderma that fail to respond to initial therapy with antibiotics should not be assumed to have MRSP. Empiric choice of a so-called stronger antibiotic, particularly a drug reserved for proven MRSP, is strongly discouraged, as this may result in a multidrug-resistant infection. Antibiotic choice should be based on results of culture and sensitivity testing.

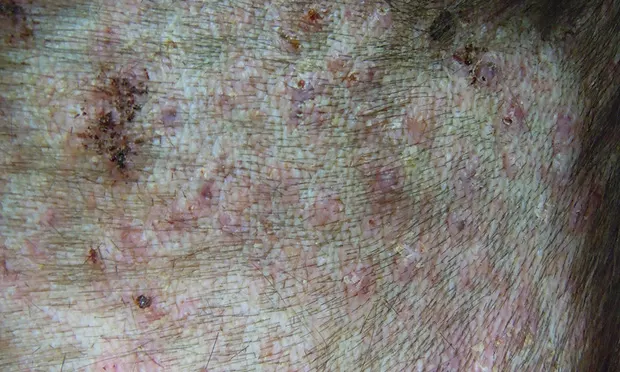
Bacterial infection by MRSP in a 10-month-old male springer spaniel
Samples for culture are best obtained when previous antibiotic therapy (and topical antiseptic therapy) has been discontinued for several days. Exudate from within a pustule or from beneath the peeling edge of an epidermal collarette is preferred for culture.
Based on culture and sensitivity testing results, potentiated sulfonamides at 15–30 mg/kg q12–24h and chloramphenicol at 30–50 mg/kg q8–12h are common treatment options. Additional choices—if reported effective—may include clindamycin at 11 mg/kg q24h or doxycycline at 5–10 mg/kg q12–24h. In cases with multi-drug resistance, amikacin at 20 mg/kg q24h or rifampin at 10 mg/kg q12–24h may be required. However, these antibiotics are associated with potentially life-threatening effects; clients should be counseled on adverse reactions and the need for proper laboratory monitoring. Treatment should continue until one week past clinical resolution of all regions.
Topical antiseptic therapy is critical. Patients with MRSP should be bathed twice weekly, even daily if possible. Shampoos containing 2%–4% chlorhexidine or 2.5%–3% benzoyl-peroxide have demonstrated excellent efficacy. Conditioners and sprays containing chlorhexidine and dilute (5%) household bleach solution rinses provide excellent residual antiseptic effects.
Environmental decontamination may help reduce recolonization with MRSP. Household bleach at a 1:32 dilution is bactericidal for MRSP.
SPECIAL CONSIDERATIONS
When treating MRSP, clients should avoid contact with the infected area of the patient, and especially discourage licking of the face or any area of damaged skin. Avoidance of areas most commonly colonized by MRSP (lips, nose, anus) is advised.
Related ArticleMRSP Infections: Addressing Common Client Questions
Contact with the patient should be followed by hand washing or the use of an alcohol-based hand sanitizer, especially for an immune-compromised individual.
Infected patients should not be in contact with other animals, and should not go to day care, groomers, or dog parks. While concurrent colonization of humans and pets with MRSP has been reported, transmission of infection is rare. MRSP may not be contagious, but exposure of potentially susceptible individuals should be avoided.
Feces can be colonized by MRSP. Prompt removal of waste and frequent cleaning of litter boxes reduce environmental contamination.
Environmental clean-up should include frequent washing of bedding, toys, and bowls. Pets should not sleep in the client's bed until the infection has resolved.
Primer
Alexander Werner, VMD, DACVD, Animal Dermatology Center, Studio City, California
MRSA & MRSP By the Numbers
S pseudintermedius can be cultured from the skin of many healthy dogs and some cats.1
Approximately 20%–30% of humans are either intermittently or persistently colonized (subclinically) with S aureus in the nares.2
The frequency of isolating MRSP from infections, especially from pyoderma, has changed dramatically in the past 15 years. Studies of isolates from as recently as 2000 demonstrated little resistance to either cephalexin or fluoroquinoles, whereas in a 2009 follow-up study, resistance increased to 10% and 30%–40%, respectively.1
The greatest risk for MRSP development is prior treatment (within one year) with antibiotics.
MRSP is reported to colonize 4.5% of healthy dogs and 1.2% of healthy cats.3
Nasal carriage of MRSP in veterinary professionals was reported in one study to be 3%–5.3%.4,5 Owners of pets with MRSP had a carriage rate of 4%–13%.6,7 Repeat cultures from 2 owners were negative following treatment of their pets.5
MRSA is reported to colonize up to 3.5% of the general human population.8
MRSP can contaminate the environment. MRSP can be isolated in samples from 5%–10% of veterinary practices and from the environment 6 months after clinical resolution of an infected animal.8
S pseudintermedius typically colonizes dogs and cats and is transient in humans; S aureus typically colonizes humans and colonizes (and infects) dogs poorly. Decolonizing dogs and cats of staphylococci is likely impossible.
Canine pyoderma caused by MRSA is almost always associated with human MRSA infection in the immediate environment. Colonization by MRSA in dogs is rapidly lost following treatment of the human source for infection and/or removal from potentially contaminated environments (eg, hospital, nursing home).
Related ArticleMRSP is Not MRSA
Communication
Christopher Keller, Animal Dermatology Center, Studio City, California
A key to resolving MRSP infections is client compliance. While treatment may seem demanding initially, the quickest way to resolve the infection is to follow all recommendations.
Discuss Oral Antibiotics
Appropriate antibiotics will be prescribed to resolve the infection and may need to be continued for extended periods of time. Team members should remind clients to give the medication as directed, and for the entire period prescribed, to avoid developing more resistance. As with any new medication, clients should be advised of possible adverse effects and instructed to call with any questions or concerns.
Related ArticleMRSP Infections: Addressing Common Client Questions
Technician: Mrs. Smith, the veterinarian is starting Lucy on oral antibiotics to clear the infection. It is very important that you give these medications as directed. You will be continuing the antibiotics even after all the signs of the infection have resolved, so don’t discontinue the medications just because Lucy looks healed, which could lead to an even more resistant infection. The veterinarian may request a recheck examination before completing the antibiotics.
Discuss Topical Therapy
Treatment will also include frequent topical therapy (eg, antiseptic shampoos, conditioners, rinses, sprays). The team should review these products and stress their importance in the treatment plan.
Technician: You will need to bathe Lucy once to twice a week. I know sometimes that can be difficult, but bathing can be very helpful and may decrease the amount of time you need to treat her. You will first wet her coat, then apply and lather the shampoo. Make sure you massage all the way down to the skin. The lather will need to stay on Lucy for 5–10 minutes, so you may want to keep a toy or a few treats handy to help her pass the time. Rinse her well, then apply the conditioner (and rinse, if prescribed).
Related ArticleClient Handout: MRSP & Your Pet
Discuss Cleaning
While it is unlikely a healthy human will acquire an MRSP infection from his or her pet, cleaning the pet’s environment is important. A 1:32 dilute bleach solution is an effective cleanser, where possible. Clients should also be advised to wash their hands frequently, especially after handling their pet.
Technician: Cleaning Lucy’s living areas would be very helpful. Wash her bedding, food and water bowls, and toys often. Use a dilute bleach solution (a 1:32 ratio, or 1/2 cup per gallon of water). While it would be very unlikely for this infection to spread to a healthy human, you should wash your hands after contact with Lucy (bathing, medicating, playing). Finally, you should keep her away from social activities (dog parks, groomers, day care) until the infection has cleared.
Workflow
Christopher Keller, Animal Dermatology Center, Studio City, California
Each team member can gather vital information from the client that will shape a patient’s individual treatment plan. The team workflow below can help make your practice more effective in addressing patients with methicillin-resistant Staphylococcus pseudintermedius—from client interaction to proper precautions and treatment-plan compliance.
1 Receptionist
Welcome the client.
Separate a patient with previously diagnosed MRSP from other patients, possibly by moving them immediately into an examination room.
Clean areas the patient has contacted with antiseptic cleanser.
Wash hands after handling the patient.
2 Veterinarian
Devise a formal infection-control program that will guide team members on how to address concerns when a patient known to have MRSP comes into the practice. Collect input from all members of the team (veterinarians, technicians, assistants, receptionists) because they all will see this from different aspects according to their roles.
Review the patient’s history, discuss current problems, and perform a complete physical examination.
Discuss diagnostic testing, steps taken after testing, a tentative diagnosis, and a treatment plan with the client.
Advise the client of the recommended recheck schedule.
Make sure all of the client’s questions are answered.
Wash hands after handling the patient.
3 Technician/Assistant
Keep the MRSP patient separated from other patients.
Collect necessary laboratory samples (skin smears, cultures, blood samples).
Prepare medications, shampoos, conditioners, rinses, and/or sprays.
Discuss treatment with the client, stressing the importance of following recommended protocols.
Discuss environmental cleaning and the need for good hygiene.
Answer any additional client questions.
Clean areas the patient has contacted with antiseptic cleanser.
Wash hands after handling the patient.
4 Receptionist
Provide the client with an invoice.
Schedule a recheck examination.
5 Technician/Assistant
Make follow-up calls to the client, discuss any new laboratory results, and answer any new questions the client may have.
Roles
Christopher Keller, Animal Dermatology Center, Studio City, California
Every practice team member plays an important role in diagnosing and treating diseases. Following are each member’s roles and responsibilities when addressing MRSP infection.
Clean contaminated areas with antiseptic solutions (ie, dilute bleach).
Make staff aware of the patient’s presence to maintain separation and proper infection control.
Follow all contact with the patient with hand washing and/or the use of an alcohol-based hand sanitizer.
| | TECHNICIAN/ASSISTANT | Client educator |
Separate the patient as much as possible to avoid contact with other patients.
Disinfect all equipment used to treat or evaluate the patient with dilute bleach or an alcohol-containing cleanser.
Clean contaminated areas (including the examination room) with antiseptic solutions (eg, dilute bleach).
Change clothing prior to contact with other patients, if possible; wearing disposable gloves while handling the infected patient is useful.
| | VETERINARIAN | Medical expert and client educator |
Treat the patient as completely as you would MSSP cases.
Emphasize the need for client compliance with all aspects of treatment, including topical therapy.
Advise the client of the need for good hand and environmental hygiene, but do not make him or her panic.
Clean all equipment used to treat or evaluate the patient.
Follow all contact with the patient with hand washing and/or the use of an alcohol-based hand sanitizer.
|
Training
Christopher Keller, Animal Dermatology Center, Studio City, California
With the increasing number of MRSP infections, veterinary practices will be answering more client questions about MRSP. Make sure each team member knows the appropriate answers.
Addressing Common Client Questions
Q: What is MRSP?A: MRSP, or methicillin-resistant Staphylococcus pseudintermedius, is a bacterial infection that can cause skin infections in dogs and sometimes cats, and is resistant to many common antibiotics. It is important to keep in mind that MRSP is not methicillin-resistant Staphylococcus aureus (MRSA). MRSP rarely becomes systemic; its effects are limited primarily to infections on the skin.
Q: Can I get MRSP?A: It is unlikely that a healthy adult will get an MRSP infection from a pet. If individuals in the household have a compromised immune system, keeping the pet separated as a precaution is recommended.
Q: Is MRSP contagious to my other pets?A: Healthy pets may carry the bacteria, but they should not become infected.
Q: Can this infection be cured? Will it come back?A: The veterinarian will prescribe antibiotics based on skin culture results. You will also need to do a lot of bathing and keep your pet’s environment clean. It may be necessary to look for an underlying cause of the infection to prevent it from returning.
Review of MRSP Therapy
The entire team should be well versed on standard treatments for MRSP to educate clients on therapies. Review and discuss the following topics at a team meeting about MRSP:
Adverse effects of common antibiotics used to treat MRSP infections
Procedures for therapeutic bathing and use of topical treatments
Household hygiene techniques.
Keys to Successful Infection Control
Wash hands frequently with soap and water.
Use an alcohol-based hand sanitizer, if available.
Change uniforms after restraining an MRSP patient.
Clean and disinfect all areas and instruments that MRSP patients contact. A dilute bleach solution (1:32) is a good sanitizer; however, other commercially available products may be available. Be sure to check the label for necessary concentration and contact time.
Keep known MRSP patients separated from other patients.
Handout
Alexander Werner, VMD, DACVD, Animal Dermatology Center, Studio City, California
You are likely aware of MRSA, a type of staph infection that has become resistant to treatment with commonly used antibiotics. You may be confused, then, if you hear your dog or cat has been infected with MRSP. Do not worry—although the 2 bacteria have similar names, they are different organisms and MRSP does not pose the threat to human—or pet—health that MRSA does.
While multiple antibiotic-resistant bacterial infections are becoming more of a problem in both human and animal medicine, they are treatable. Staphylococcus pseudintermedius (SP), the most common cause of bacterial skin infection in dogs, may temporarily colonize (remain without causing harm) human skin, but should not cause problems in healthy individuals.
Related ArticleMRSP Infections: Addressing Common Client Questions
Can HUMANS Catch MRSP? Can Other Pets?
Other than from dog bites, MRSP infection in humans is very uncommon. The zoonotic risk (the chance of transmission of an infection from animal to human) is low, but individuals with compromised immune systems may be at higher risk.
Other dogs can be colonized with MRSP from an infected or colonized dog. However, for infection to develop, skin damage and/or immune compromise must be present in the exposed animal. Still, it is prudent not to expose other animals to dogs known to be infected. Quarantine of the animal entirely is probably not necessary, but avoiding dog parks, day care, and grooming shops during treatment is advisable.
Listen to Your Veterinarian
As for treatment of all diseases in companion animals, strict adherence to the veterinarian’s recommendations is very important. This is especially true for treatment of MRSP. Discontinuing antibiotics before finishing the full course prescribed only encourages the return of infection, possibly with resistance to a previously effective drug. In addition, the search for and control of any underlying problem (such as an allergy) that encouraged the development of MRSP is necessary.
Treatment must include topical therapy for the skin irritation, such as bathing with an antiseptic shampoo and the application of antiseptic rinses. This not only increases patient comfort and hastens healing, but also decreases environmental contamination and the potential exposure of noninfected individuals in the household (including animals and humans).