Calcium Oxalate Urolithiasis

You have asked…
How should I manage calcium oxalate urolithiasis?
The expert says…
The overall prevalence of calcium oxalate (CaOx) uroliths in dogs has increased significantly over the past 10 years.1 This may be associated with increased use of acidifying diets; changes in dietary content of calcium, magnesium, phosphorus, and oxalate; more sedentary lifestyles; decreased water intake; increased ownership of small breeds more prone to developing CaOx uroliths; increased incidence of overweight dogs; and/or dogs living to more advanced ages.1,2
Related Article: Calcium Oxalate Crystalluria
Approximately 70% of canine CaOx uroliths submitted to the Canadian Veterinary Urolith Centre between 1998 and 2008 were from male dogs; commonly affected breeds included the miniature and standard schnauzer, miniature poodle, Yorkshire terrier, Lhasa apso, bichon frise, and shih tzu. Female miniature schnauzers appear to be a gender exception; in one study, they developed CaOx uroliths more frequently than struvite uroliths.1 The overall increased prevalence in male dogs may be related to an increase in the hepatic production of oxalate mediated by testosterone. Conversely, estrogens in female dogs may increase the urinary excretion of citrate, which facilitates the formation of soluble calcium citrate.2
Many cats with CKD also have CaOx nephroliths.
Similar to dogs, male cats most commonly develop CaOx uroliths. Male domestic short-haired, medium-haired, and long-haired cats appear to be 1.4 times more likely to develop a CaOx urolith than a struvite urolith.1 Both male and female purebred cats (eg, the Persian, Himalayan, Burmese, ragdoll) appear to be at risk.1 Many cats with chronic kidney disease (CKD) also have CaOx nephroliths, although it can be difficult to differentiate small CaOx nephroliths from renal soft-tissue mineralization. Over the past 10 years, submission of feline CaOx uroliths has been constant, while the submission of feline struvite uroliths has declined.1
Figure 1A. Lateral radiograph of a 13-year-old, castrated shih tzu with multiple CaOx uroliths (kidneys, bladder, and urethra).
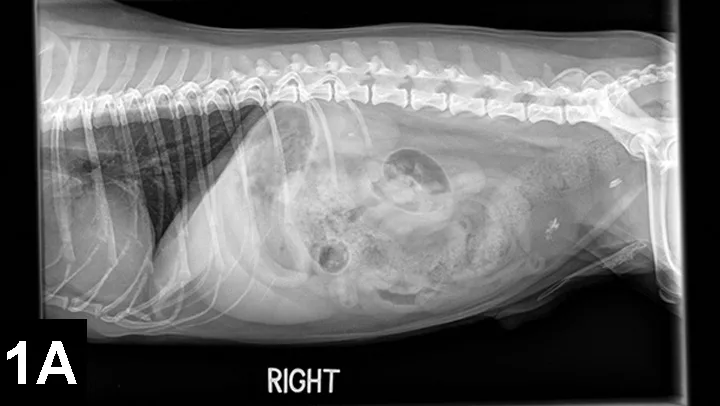
Figure 1B. Tucked lateral radiograph showing additional CaOx urethroliths

Older dogs and cats (8–12 years) are most commonly affected by CaOx uroliths, and concurrent urinary tract infection appears to be rare. CaOx uroliths are typically the most radioopaque of all uroliths and usually easily observed on plain film radiographs (Figures 1 and 2).
Figure 2. Lateral radiograph of a 9-year-old, castrated domestic long-haired cat with suspected CaOx nephroliths and a single CaOx urocystolith).

Pathophysiology
CaOx uroliths are most commonly the monohydrate form (crystal name, whewellite) rather than the dihydrate form (weddellite; Figure 3).
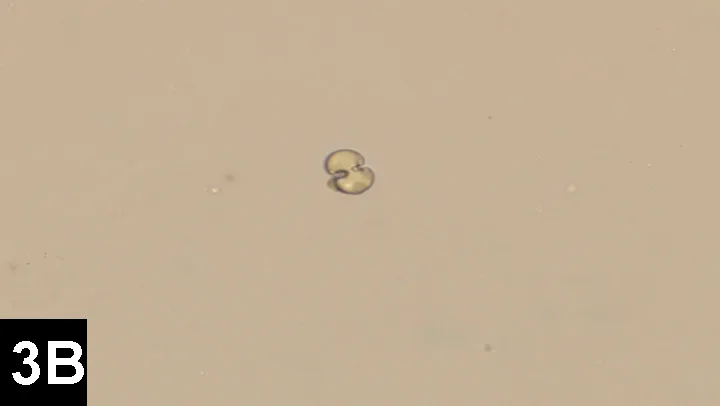
Figure 3. Monohydrate and dihydrate CaOx crystals. Images courtesy of Dr. Lisa Pohlman
The factors involved in the pathogenesis of CaOx urolithiasis in dogs and cats are not completely understood but, at least in part, involve urine supersaturation with calcium and oxalate. CaOx solubility is increased in urine with a pH >6.5, whereas a urine pH of <6.5 tends to favor CaOx crystal formation. CaOx uroliths may have sharp protrusions (Figures 4 and 5).
Hypercalciuria is most likely to occur in dogs postprandially associated with increased absorption of calcium from the gut. Hypercalciuria may also occur secondary to overt hypercalcemia (eg, primary hyperparathyroidism, neoplasia, vitamin D intoxication, idiopathic hypercalcemia). Ionized calcium concentrations should be measured in dogs and cats with CaOx uroliths to rule out hypercalcemia. Another potential cause of hypercalciuria is defective tubular reabsorption of calcium resulting in normocalcemic hypercalciuria; a third cause is excessive demineralization of bone, which releases calcium and phosphorus in the bloodstream. All these mechanisms may be interrelated. For example, impaired tubular reabsorption of calcium stimulates production and release of parathyroid hormone, which can increase intestinal absorption of calcium and release of calcium from bone.
Figure 4. 95% CaOx monohydrate and 5% CaOx dihydrate uroliths from the dog in Figure 1 (scale, 1 division = 1 mm).
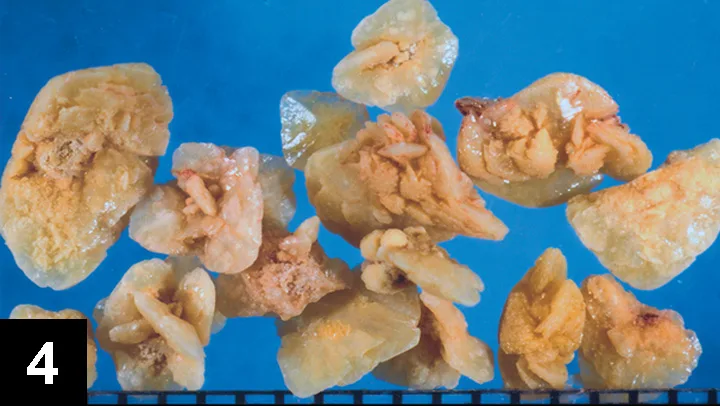
Figure 5. 100% CaOx monohydrate urocystolith from a cat (scale, 1 division = 1 mm).

Treatment with certain drugs (eg, glucocorticoids, furosemide) or dietary supplementation with calcium or sodium chloride may also result in hypercalciuria. An association between hyperadrenocorticism and the development of calcium-containing uroliths has also been identified in dogs.3 Decreased urine concentrations of glycosaminoglycans, Tamm–Horsfall protein, osteopontin, and/or citrate, all of which which are CaOx crystallization inhibitors; defective urinary nephrocalcin (another CaOx crystallization inhibitor); or increased dietary intake of oxalate (eg, vegetables, grass, vitamin C) may increase the risk for CaOx urolith formation in dogs.4 In rodents and humans, decreased concentrations of oxalate-degrading bacteria like Oxalobacter formigenes in the gut appears to be a risk factor for CaOx urolith formation; the same may be true for dogs and cats.4 Obesity may also increase the risk of CaOx urolithiasis in dogs.2
|
Hypercalcemia
Defective tubular reapsorption of calcium
Excessive demineralization of bone
Dietary supplementation with calcium or sodium chloride
Some drugs (eg, glucocorticoids, furosemide)
Decreased urine concentrations of glycosaminoglycans, Tamm-Horsfall protein, osteopontin, and/or citrate
Defective urinary nephrocalcin
Increased dietary intake of oxalate
Decreased concentrations of oxalate-degrading bacteria like Oxalobacter formigenes in the gut
Hyperadrenocorticism
Metabolic acidosis
|
Recurrence for CaOx uroliths in dogs is relatively high and appears to be higher than in cats. In one study, CaOx uroliths recurred following surgery in 3% of dogs by 3 months, 9% by 6 months, 36% by 12 months, and 48% by 24 months.5 In another study of more than 2000 cats with CaOx uroliths, 7% had a first recurrence, 0.6% had a second recurrence, and 0.1% had a third recurrence.6 These results underscore the need for medical protocols aimed at decreasing the recurrence of CaOx uroliths after urolith removal.
Treatment
Medical treatment for the dissolution of CaOx urolithiasis has not yet been developed. Surgical removal of urocystoliths remains the primary treatment modality, although less invasive urolith retrieval and/or destruction methods (eg, voiding urohydropropulsion, catheter retrieval, stone basket retrieval, lithotripsy) are becoming more commonplace.
Medical protocols aimed at decreasing the recurrence of CaOx uroliths after urolith removal are critical.
In cases of suspected CaOx nephrolithiasis, surgery is usually not indicated unless there is an obstructive uropathy, uncontrolled infection, or deteriorating renal function. In cats with CKD and suspected CaOx nephroliths, there appeared to be no increased risk for kidney disease progression, uremic crises, or death compared with cats with similar stage CKD without nephroliths.7 Patients with nephroliths should be managed with medical protocols designed to prevent or slow CaOx urolith growth, and the location and size of the nephroliths should be monitored radiographically or ultrasonographically several times a year. Acute decompensation of a CKD patient with known or suspected nephroliths should prompt swift evaluation to rule out an obstructive uropathy.
|
Male gender
Middle to older age
Consumption of human foods with high calcium and/or oxalate content
Hypercalcemia
Certain breeds
|
Medical Management for Prevention
Patients should be carefully assessed for factors that can increase calcium and oxalate supersaturation. Because hypercalcemia can cause hypercalciuria, ionized calcium concentrations should be assessed in dogs and cats with known or suspected CaOx uroliths. In addition, increased urinary calcium excretion has been associated with hyperadrenocorticism, exogenous glucocorticoid administration, and metabolic acidosis, and, therefore, these conditions should be ruled out when appropriate.
The mainstays of medical management include encouraging water intake to achieve a urine specific gravity <1.020 in dogs and <1.030 in cats (which can be challenging) and managing dietary intake to reduce hypercalciuria and hyperoxaluria. Canned diets are usually recommended over dry diets because of their high water content. Moderate restriction of protein, calcium, oxalate, and sodium intake in association with normal intake of phosphorus, magnesium, and vitamins C and D is recommended to prevent recurrence of CaOx uroliths after surgical removal.8 Hill’s Prescription Diet u/d Canine Non-Struvite Urinary Tract Health (hillsvet.com) and Royal Canin Veterinary Diet Urinary SO (royalcanin.us) are usually recommended for dogs; Hill’s Prescription Diet c/d Multicare Feline, Royal Canin Veterinary Diet Urinary SO, Purina UR Urinary St/Ox Feline Formula (purinaveterinarydiets.com), and Iams Veterinary Formula Urinary-O Plus Moderate pH/O (iams.com) are recommended for cats. Increased dietary sodium intake may result in an increase in the urinary excretion of calcium and should be avoided. Feeding human foods with high calcium and/or oxalate content (eg, chocolate, peanuts, beets, sweet potatoes, spinach, rhubarb) should be avoided.
Related Article: Nutritional Management of Urolithiasis
Oral potassium citrate may help prevent recurrence of CaOx uroliths as citrate complexes with calcium, thereby forming the more soluble calcium citrate in urine. In addition, potassium citrate results in mild urine alkalization, which increases the solubility of CaOx.4 Overzealous urine alkalization should be avoided, however, as it may result in the formation of calcium phosphate uroliths. Urine alkalization is indicated if the urine pH is consistently below 6.5. Potassium citrate should be titrated to produce an ideal target urine pH of 7.0 to 7.5. The recommended starting dose of potassium citrate is 40 to 75 mg/kg PO q12h. Thiazide diuretics have also been recommended to decrease the urinary excretion of calcium in dogs and cats with recurrent CaOx urolithiasis; hydrochlorothiazide (1–2 mg/kg PO q12h for 2 weeks) has been shown to reduce urine calcium excretion in dogs.9 This effect was enhanced by combining treatment with Hill's Canine Prescription Diet u/d.
The use of thiazide diuretics in dogs should not be a first-line treatment. Long-term use of thiazides to prevent recurrence of CaOx uroliths in dogs has not been evaluated. In healthy young female cats, hydrochlorothiazide was associated with lower urine CaOx saturation but no difference in 24-hour urine calcium excretion.10 The author cautions that the results of this study should not be extrapolated to cats that form CaOx uroliths.
|
Rule out hypercalcemia.
Hypercalciuria has been associated with hyperadrenocorticism, glucocorticoid treatment, furosemide treatment, and metabolic acidosis.
Avoid calcium-containing supplements and high-calcium foods (eg, peanuts, chocolate).
Feed canned, protein-reduced diets that alkalinze the urine (eg, Hill's Prescription Diet u/d).
Supplement potassium citrate if urine pH is not consistently >7.0.
|
CaOx = calcium oxalate, CKD = chronic kidney disease
GREGORY F. GRAUER, DVM, MS, DACVIM, is professor and Jarvis chair of medicine in the department of clinical sciences at Kansas State University. His area of interest, research, and teaching is the small animal urinary system, a topic about which he lectures at the NAVC Conference. He has served as professor and section chief of small animal medicine at Colorado State University and faculty member at University of Wisconsin–Madison, where he completed his internship and residency and earned his MS. Dr. Grauer earned his DVM from Iowa State University.