Clinical Signs of Anterior Uveitis in Dogs & Cats
Andrew Christopher Lewin, BVM&S, DACVO, University of Tennessee
Renee Carter, DVM, DACVO, Louisiana State University
Anterior uveitis is common in veterinary medicine and refers to inflammation of the iris and ciliary body. The posterior uvea may also be involved (ie, panuveitis, which is inflammation of both the anterior and posterior uvea).1 Diagnosis can be challenging due to the variety of disease presentations.
Clinical signs may include ocular discomfort (eg, blepharospasm), epiphora, aqueous flare, corneal edema, hyphema, hypopyon, fibrin clot formation, keratic precipitates, posterior synechiae, iridal hyper- or depigmentation, conjunctival hyperemia, episcleral congestion, and corneal neovascularization. Patients often have low intraocular pressure (<10 mm Hg).
The underlying cause of anterior uveitis should be investigated. Some cases have a local cause (eg, infected corneal ulcer, foreign body, cataract). Lens-induced uveitis is more common in dogs. When the underlying cause is not apparent, a general, systemic diagnostic examination is indicated and should include CBC, serum chemistry profile, urinalysis, infectious disease testing, coagulation testing, blood pressure assessment, ocular ultrasonography, thoracic radiography, and abdominal ultrasonography. Many cases are classified as idiopathic.
Treatment for clinical signs includes topical ocular medications with or without systemic anti-inflammatory medications and topical atropine. Comorbid conditions may preclude use of certain drugs in some patients; examples include corneal ulceration (topical steroids), glaucoma (atropine), systemic infectious disease (systemic steroids), and pre-existing conditions (eg, renal disease; systemic NSAIDs).
The following are clinical images of anterior uveitis cases.
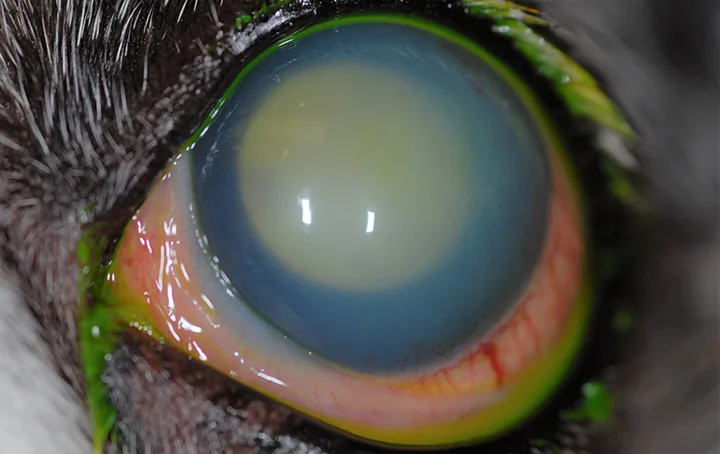
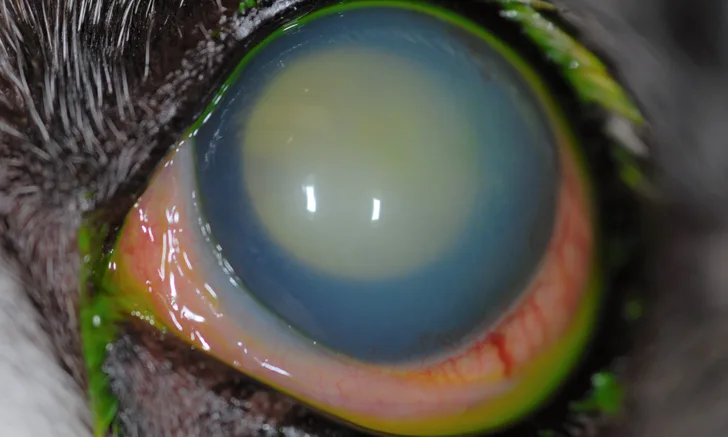
FIGURE 1
Diffuse corneal edema, conjunctival hyperemia, episcleral congestion, and decreased intraocular detail. Classic clinical signs of acute uveitis in a dog, including significant aqueous flare in the anterior chamber. Intraocular pressure was 4 mm Hg, and vision was reduced (assessed with menace response). Fluorescein dye had been recently applied.
All images are used with permission from Louisiana State University with special thanks to Dr. Melanie Mironovich.
Editor’s note: This article was originally published in December 2021 as “Clinical Signs of Anterior Uveitis.”