Abnormal Head Position in a Terrier

A 1-year-old, 1-kg, castrated Yorkshire terrier was presented for stumbling, reluctance to climb stairs, and abnormal head position.
History
According to the owner, the dog had refused to climb stairs during the past 3 weeks and had stumbled and fallen twice in the past 3 days. In addition, the owner noted that the dog’s neck appeared to be twisted, and the dog was vocalizing as if in pain. The dog’s vaccinations were up-to-date.
Examination
On examination, the dog appeared bright and alert, with a normal body temperature, pulse, and respiratory rate. Although the dog was ambulatory, ataxia was noted in all limbs, occasional scuffing of the right thoracic limb was evident, and marked torticollis was present (Figure 1, above. Marked torticollis was evident on presentation).
No cranial nerve deficits were apparent on neurologic examination. However, conscious proprioceptive and postural reaction deficits were present in all limbs and more severe in the right thoracic and pelvic limbs. Segmental spinal reflexes were normal in all limbs. Hyperpathia was detected on deep palpation of the cervical region.
Ask Yourself...
What is the neuroanatomic location of the dog’s lesion?
What are the most likely diagnostic differentials?
What initial diagnostic plan is indicated?
Diagnosis
Caudal Occipital Malformation Syndrome (COMS) and Syringomyelia (SM)
The prevalence of COMS with associated SM is high in several small and toy breeds, most notably the Cavalier King Charles spaniel.1-3 Clinical signs of COMS with SM can be variable and reflect dysfunction of the vestibular system, cerebellum, or cervical spinal cord, or they can suggest a multifocal lesion.
Dogs with SM-associated COMS often present with signs of maladaptive neuropathic pain, which may include allodynia (eg, intolerance to petting or grooming the head and neck) or dysesthesia (eg, phantom scratching of the head, neck, or shoulders without making contact with the skin).1 In theory, these behaviors arise from damage to the dorsal horn of the spinal cord or ascending nociceptive pathways caused by SM.4
Diagnostics

In this case, cervical radiographs (Figure 2) showed scoliosis (which could not be manually corrected under sedation) but no other abnormalities. MRI of the cervical spine and brain (Figure 3) was performed because of the diagnostic considerations, clinical severity, and progressive nature of the signs.
COMS, or Chiari-like malformation, is a developmental abnormality principally defined by occipital hypoplasia causing overcrowding of brain structures contained within the caudal fossa.1,5 This results in flattening of the caudal aspect of the cerebellum and cerebellar herniation into or through the foramen magnum (Figure 3, white arrowheads), medullary kinking (red arrow), and obstruction of the flow of cerebrospinal fluid (CSF) in the dorsal subarachnoid space at the craniocervical junction (white arrowheads).
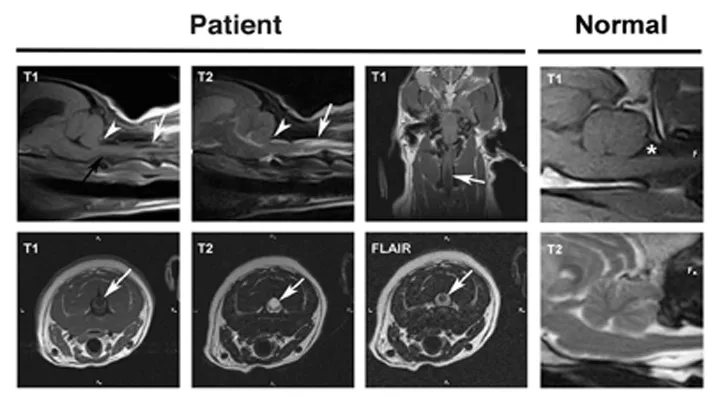
SM is characterized by the development of fluid-filled cavities within the spinal cord parenchyma and can be caused by numerous congenital (Figure 3, white arrows) or acquired (eg, trauma, meningitis, neoplasia) mechanisms of disturbed CSF flow dynamics.1,2,5
In normal dogs (Figure 3, far right panel), the caudal aspect of the cerebellum has a rounded appearance and does not encroach on the foramen magnum. The dorsal subarachnoid space is prominent at the craniocervical junction (white and red asterisks), and there is no medullary kinking.
Clinical signs are more common in dogs with SM-associated COMS, and there may be some correlation between severity of SM and severity of clinical signs. COMS, both with and without associated SM, may also be an asymptomatic incidental finding in at-risk breeds.5
Management
The primary goals of multimodal medical therapy (see Treatment at a Glance, below) are to slow disease progression by decreasing CSF production and palliating neuropathic pain.4 Because COMS with SM is a mechanically obstructive problem, corrective surgery (often involving decompression of the foramen magnum and variably extensive cervical dorsal laminectomy) offers a better chance for long-term control of clinical signs.3
Although the indications for and timing of surgical intervention are controversial—especially in asymptomatic or mildly affected dogs—many neurologists advocate surgery in dogs that do not respond to medical therapy, have severe or progressive clinical signs, or have early-age onset of clinical signs.
Some dogs require adjunct medical therapy to control clinical signs following surgery. As a result of constrictive membrane (scar) formation at the surgical site, clinical signs can recur or new signs develop several months to years after surgery.3
Outcome
In this case, the dog’s pain responded to treatment with prednisone, gabapentin, and furosemide; however, both the torticollis and tetraparesis worsened. Following decompression of the foramen magnum 6 weeks after initial evaluation, all clinical signs (except persistently mild torticollis) had resolved.
Did You Answer?
1. The findings were consistent with a neuroanatomic diagnosis of a cervicothoracic (C1–T2) myelopathy, as there were deficits in all limbs, preservation of spinal reflexes, cervical pain, and no evidence of deficits referable to an intracranial lesion. Because no appreciable spinal reflex changes were evident, further characterization of the lesion as affecting the C1–5 or C6–T2 spinal segments was impossible.
2. The most likely differentials are congenital malformations—COMS, atlantoaxial instability, SM, meningomyelitis, and diskospondylitis. Intervertebral disk disease and spinal tumors rarely occur in dogs of this age.
3. Survey radiography of the cervical spine under sedation is indicated to rule out atlantoaxial instability and diskospondylitis.
Tx at a Glance
Reduction of CSF Production
Furosemide: 0.5–1 mg/kg PO q12–24h
Acetazolamide: 5–10 mg/kg PO q8–12h
Omeprazole: 0.5–1 mg/kg PO q24h
Neuropathic Pain-Modifying Agents
Gabapentin: 5–15 mg/kg PO q8–12h
Amantadine: 3–5 mg/kg PO q24h
Antiinflammatory Drugs (Note: These drugs should not be prescribed concurrently)
Prednisone: 0.5 mg/kg PO q12–24h
Carprofen: 2.2 mg/kg PO q12h
JOHN H. ROSSMEISL, JR, DVM, MS, DACVIM (SAIM & Neurology), is an associate professor of neurology and neurosurgery at the Virginia-Maryland Regional College of Veterinary Medicine in Blacksburg, Virginia. Dr. Rossmeisl’s research interests include molecular biology and therapy of CNS tumors, as well as neurologic complications of endocrine diseases. He delivered CE lectures at the NAVC Conference 2008 and 2011. Dr. Rossmeisl earned his DVM and completed residency programs in small animal internal medicine and neurology at Auburn University.